JAMA Oncol:谢丛华教授发现肿瘤患者感染新冠病毒的风险是普通人群的2.31倍
2020-03-27 张玉辉 医师报
3月25日,国际医学期刊《JAMA Oncology》在线发表了由武汉大学中南医院肿瘤放化疗科谢丛华教授及团队针对肿瘤患者新冠肺炎感染风险的一篇文章
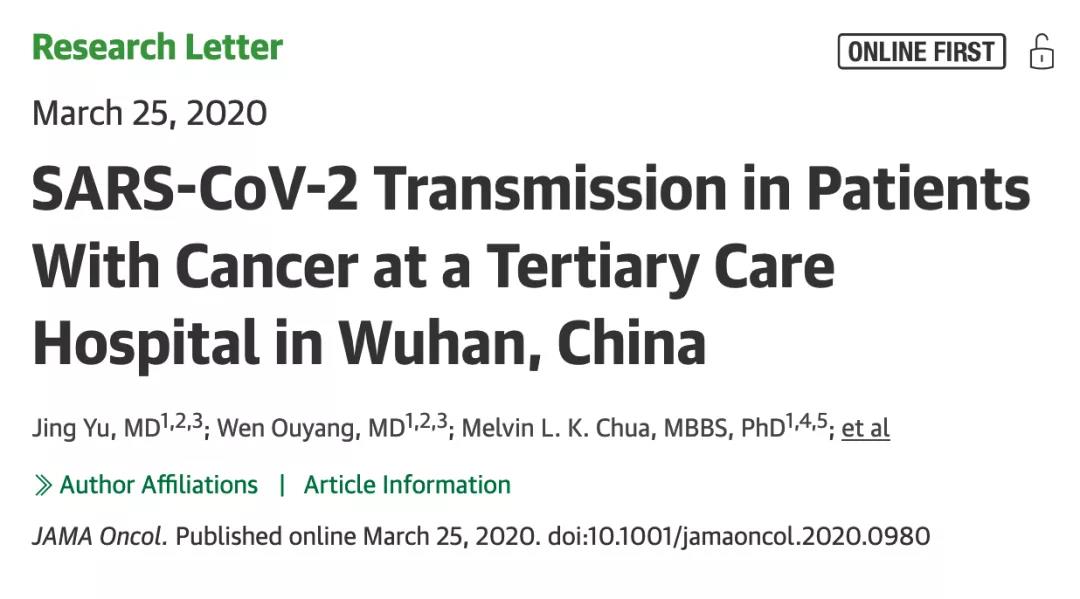
3月25日,国际医学期刊《JAMA Oncology》在线发表了由武汉大学中南医院肿瘤放化疗科谢丛华教授及团队针对肿瘤患者新冠肺炎感染风险的一篇题为《SARS-CoV-2 Transmission in Patients with Cancer at a Tertiary Care Hospital in Wuhan》的回顾性分析。
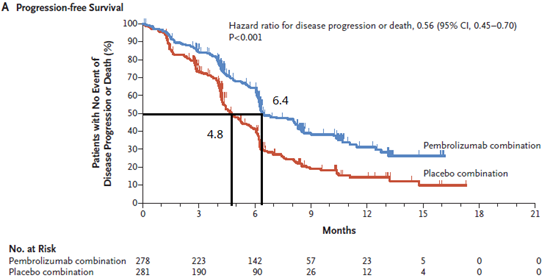
研究结果显示,暴发城市中的肿瘤患者感染新冠病毒的风险是普通人群的2.31倍。
研究主要分析了2019年12月30日~2020年2月17日在该中心住院的1524例肿瘤患者感染新型冠状病毒肺炎的风险,共纳入12例感染新冠肺炎的肿瘤患者,结果显示,肿瘤患者新冠肺炎感染率为0.79%,高于在数据截止当日武汉市的整体新冠肺炎感染率,肿瘤患者感染新冠肺炎的风险是普通人群的2.31倍。
在本组感染的肿瘤患者中,7例患者为非小细胞肺癌,其中5例正在接受治疗(化疗,化疗±免疫治疗或放疗)。截止至3月10日,12例患者中6例出院,3例仍在接受住院治疗,另外3例患者死亡。
值得注意的是,感染患者中,仅一半不到的患者正在接受抗肿瘤治疗,因此肿瘤治疗导致的免疫抑制在新冠肺炎感染中的作用值得进一步探讨,肿瘤患者定期返院治疗与随诊才是最大的感染风险。
另外,本研究中感染患者的中位年龄为66岁,进一步分析提示:年龄>60岁的患者感染风险可能高于<60岁的患者。
本研究作为疫区内,首篇针对癌症患者感染风险的原创性研究,其结果也再次印证了2020年2月发表的全国的多中心调查的结果,即癌症患者尤其是肺癌患者较普通人群具有更高的感染风险。
由于疫情的持续发展,国内外已有近47万的确诊病例(截止至2020-3-26),越来越多的国家或地区成为新的新冠肺炎爆发地,新冠病毒肺炎目前已经成为全球热门的话题。
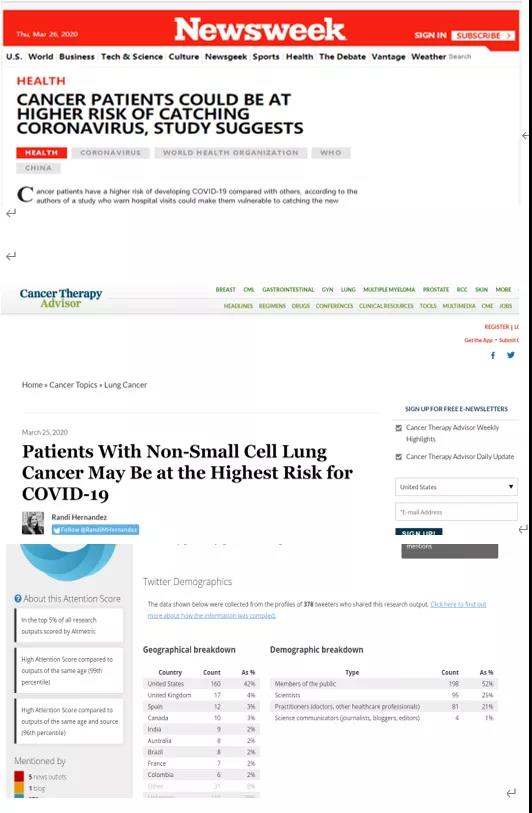
本研究在线发表后立即受到国际媒体的普遍关注,研究结果受到多家国外媒体及网络平台转载
谢丛华教授及团队指出,对于肿瘤患者,疫情期间,应该降低返院复查随诊的频率,开展线上随诊;对于一般状况比较好的患者,可适当推迟治疗以减少感染发生的风险;对于需要治疗的患者,必须在适当的隔离条件下进行,以降低SARS-CoV2的感染风险。
该结果为目前正处于疫情暴发过程中的其他国家的肿瘤患者提供了治疗指导。他们希望通过这个研究结果引起社会各界对肿瘤患者的重视,尤其是疫情期间,他们是更需要关注的一群人。
原始出处:
Jing Yu, Wen Ouyang, Melvin L. K. Chua, Conghua Xie. SARS-CoV-2 Transmission in Patients with Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol.2020Mar 25.doi:10.1001/jamaoncol.2020.0980
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Oncol#
70
#肿瘤患者#
83
#普通人群#
60
新冠肺炎,疫情何时才能消失
82
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
82
谢谢梅斯分享这么多精彩信息
0