Nature平息百年淋巴管起源争议
2015-05-22 佚名 生物通
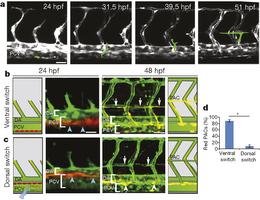
一百多年以来,科学家们一直在为淋巴系统起源这一问题争论不休——淋巴系统是血管的一个并行系统,其充当了从免疫细胞、脂肪分子到癌细胞机体内的一切物质的通道。现在Weizmann研究所生物调控系的Karina Yaniv博士解决了这一问题。在发表于5月20日《自然》(Nature)杂志上的一项研究中,她和研究小组揭示了淋巴系统在胚胎中发挥的机制,并第一次成功在实验室中培育出了淋巴细胞。一些科学家曾宣称,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








这篇文章有一定深度
83
是一篇不错的文章
117
#Nat#
72
厉害
115
牛
127
厉害
157
#淋巴管#
61
学习~~
48
Zan
122
牛逼!
113