ESC Heart Failure:非侵入性方法测量慢性心力衰竭患者身体成分结果比较
2021-07-04 MedSci原创 MedSci原创
恶病质(cachexia)亦称恶液质。表现为极度消瘦,皮包骨头,形如骷髅,贫血,无力,完全卧床,生活不能自理,极度痛苦,全身衰竭等综合征,在慢性心力衰竭 (CHF)患者 中很常见,
恶病质(cachexia)亦称恶液质。表现为极度消瘦,皮包骨头,形如骷髅,贫血,无力,完全卧床,生活不能自理,极度痛苦,全身衰竭等综合征,在慢性心力衰竭 (CHF)患者 中很常见,患病率为5%到15%。然而,由于细胞外液的变化,检测CHF患者的恶病质尤其具有挑战性。

pixabay
近日,发表在ESC Heart Failure杂志的一项研究通过双能 X 射线吸收仪 (DEXA) 和多频生物电阻抗分析 (BIA) 设备测量了身体成分。研究人员评估了平均年龄为70岁的120名CHF患者的身体成分。植入心脏除颤器或起搏器的患者被排除在外,因为此类患者禁用生物电阻抗测量。不能平躺或超过 DEXA 机器 150 公斤体重限制的患者也被排除在外。所有患者在同一天进行两次身体成分评估,其中还包括完整的心血管临床病史和检查、血液检查、心电图和超声心动图等。

结果显示,BIA测量的平均脂肪量 (FM) 为 27.2 (11.7) kg,而DEXA测量的FM为32.3 (12.2) kg。BIA 的平均 (SD) 瘦体重 (LM) 为 56.6 (10.9) kg,而DEXA 为 51.1 (9.9) kg。BIA测量的平均骨量(BM)为3.0(0.5)kg,而DEXA 为2.8(0.6)kg。DEXA和BIA身体成分测量与其他身体尺寸测量(身体质量指数、臀围和腰围)都有很好的相关性。
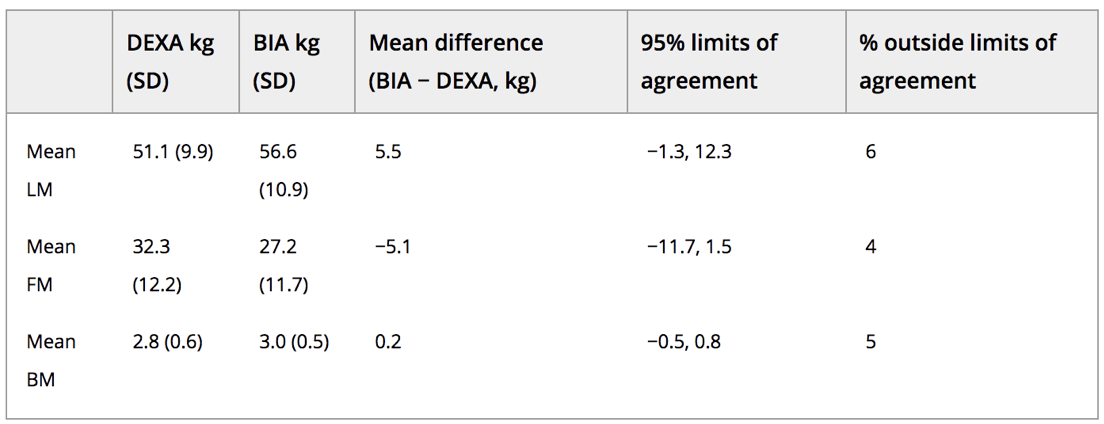
BIA 和 DEXA 测量的身体成分
该研究结果证实并扩展了其他科学家将DEXA 与 BIA 进行比较的结果。用于评估身体成分的设备不可互换。尽管 DEXA 是一种辐射源,但它仍是人体成分分析的参考方法。BIA 设备可以在门诊就诊的同时快速评估身体成分,可能更方便,但需要在恶病质研究中进一步验证。
总之,DEXA 与 BIA两种技术在 FM、LM 和 BM 的测量上存在差异,不应互换使用。
原始出处
Parin Shah.et al.A comparison of non-invasive methods of measuring body composition in patients with heart failure: a report from SICA-HF.ESC Heart Failure https://doi.org/10.1002/ehf2.13402
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非侵入性#
74
#failure#
77
#侵入性#
92
#慢性心力衰竭#
108
#ART#
70
#身体成分#
69
#HEART#
66