Cell子刊:脂质代谢或是攻克癌症复发和转移的新靶点
2017-01-06 生物探索 生物探索
导读:癌症干细胞是指具有干细胞性质的癌细胞,它具有“自我复制”以及“多细胞分化”等能力。近日,来自普渡大学、印第安纳大学医学院、西北大学的研究小组发现了对癌症干细胞功能至关重要的代谢标志。并阐述如何在卵巢癌中干预这种代谢机制以抑制肿瘤生长。这一研究发表于12月29日的Cell Stem Cell杂志上。
导读:癌症干细胞是指具有干细胞性质的癌细胞,它具有“自我复制”以及“多细胞分化”等能力。近日,来自普渡大学、印第安纳大学医学院、西北大学的研究小组发现了对癌症干细胞功能至关重要的代谢标志。并阐述如何在卵巢癌中干预这种代谢机制以抑制肿瘤生长。这一研究发表于12月29日的Cell Stem Cell杂志上。
癌症干细胞是指具有干细胞性质的癌细胞,它具有“自我复制”以及“多细胞分化”等能力。治疗癌症时如果不把癌症干细胞彻底清除,癌症很容易复发和转移,因此找到癌症干细胞,对其“斩草除根”成了攻克癌症的难题之一。近日,来自普渡大学、印第安纳大学医学院、西北大学的研究小组发现了对癌症干细胞功能至关重要的代谢标志。并阐述如何在卵巢癌中干预这种代谢机制以抑制肿瘤生长。这一研究发表于12月29日的Cell Stem Cell杂志上。
这项新研究将焦点聚集在脂肪酸去饱和过程中的关键酶上,通过抑制该酶活性从而抑制癌症干细胞的危害。“癌症干细胞中的不饱和脂质对维持其功能所需的信号传导非常重要。” 本文主要作者,普渡大学教授Ji-Xin Cheng说,“研究人员已经知道癌症干细胞在癌症发展过程中的重要意义,但脂质代谢在癌症干细胞中的作用仍然是一个非常新的研究点。理解脂质代谢在癌症干细胞中的作用为癌症检测和治疗开辟了一条新的途径。”
“在这项研究中,我们首次通过单个活细胞化学成像鉴定了卵巢癌干细胞中的不饱和脂肪。” 普渡大学博士后Junjie Li表示。他和西北大学的研究助理教授Salvatore Condello为本文的共同第一作者。
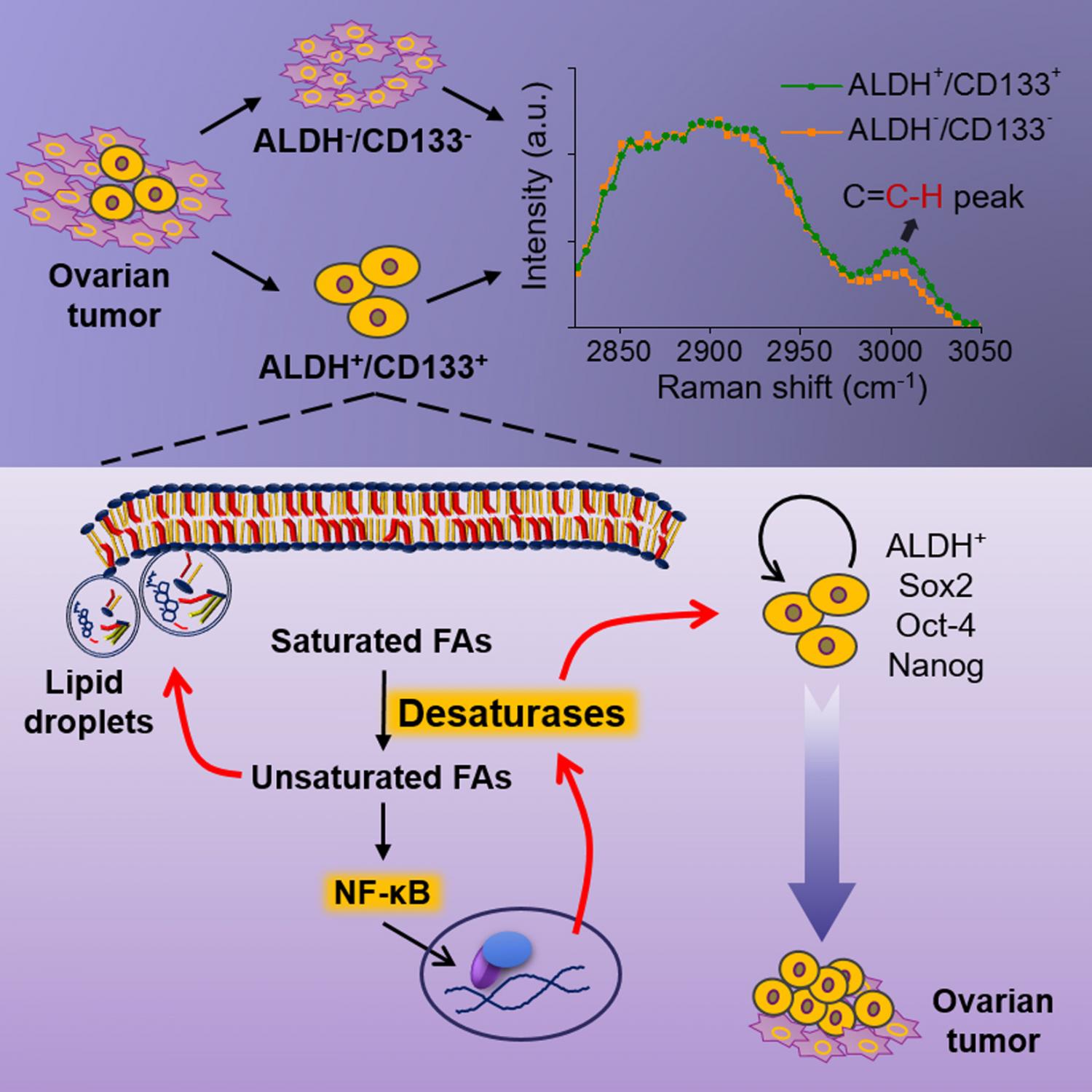
卵巢癌干细胞中不饱和脂质水平更高
研究结果显示,增加的不饱和脂肪是卵巢癌干细胞的代谢标志物,并且可能成为针对这些类型细胞的治疗靶点。在这里,研究人员提出了一种全新的策略,以根除标准治疗后诱导肿瘤复发的顽固性癌细胞,并阐明脂质代谢如何助长卵巢癌干细胞的存活。
到目前为止,由于缺乏灵敏的单细胞分析工具,癌症干细胞中代谢活性的特性研究受到限制。本研究中,研究人员开发了一种新的成像方法,并可以检测单细胞中的信号。由于癌症干细胞在癌细胞总数中所占比例很小,因而单个细胞敏感性对于检测隐藏的代谢信号至关重要。这项新方法使用两种技术:单个活细胞的高光谱受激拉曼散射成像和提取脂质的质谱分析。
“我们的研究表明,与非癌症干细胞相比,卵巢癌干细胞中的不饱和脂质水平显著增加,” Cheng表示, “传统方法不能进行单细胞分析,如果信号位于非常微小的区域,就不太容易通过常规生化检测方法观察,通过受激拉曼显微镜,我们可以通过代谢标志更好地确定这些细胞。
阻断脂质去饱和可抑制癌细胞“干性”和肿瘤发生
在实验室培养的卵巢癌干细胞和来自人类患者的细胞中均鉴定出了脂质去饱和信号。在富集癌干细胞的肿瘤球体实验室培养物中也能够检测到较高的不饱和脂水平。研究人员使用化学物质抑制去饱和酶的活性,并降低细胞的“干性”(stemness),削弱其危害性。抑制脂质去饱和酶有效地消除癌症干细胞,并抑制了实验培养物中的肿瘤球体形成,此外,在体内实验中也成功阻止实验室小鼠的肿瘤发生能力。
在进一步的机制研究中,研究人员确认核转录因子NF-κB可直接调节脂肪酸去饱和酶的生产。并抑制去饱和酶阻断NF-κB信号。
“癌症干细胞对常规治疗有抗性,并且与化疗后复发和癌症转移密切相关。”Cheng说, “了解癌症干细胞的特征和弱点将促进克服癌症复发和转移的靶向治疗更进一步发展。”
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
102
#CEL#
62
#新靶点#
119
#脂质代谢#
62
#癌症复发#
56
不知道在其他癌症中,比如肝癌中是否也这样
110