Circulation:替格瑞洛加入阿司匹林疗法不能改善冠脉搭桥术后的SVG阻塞率
2020-11-10 MedSci原创 MedSci原创
虽然使用了阿司匹林,但仍有15%的患者在冠状动脉搭桥手术(CABG)后的第一年内发生大隐静脉移植物(SVG)闭塞。POPular CABG试验探究在在CABG术后1年内,标准阿司匹林加上ticagre
虽然使用了阿司匹林,但仍有15%的患者在冠状动脉搭桥手术(CABG)后的第一年内发生大隐静脉移植物(SVG)闭塞。POPular CABG试验探究在在CABG术后1年内,标准阿司匹林加上ticagrelor(替格瑞洛)治疗是否可改善SVG的通畅情况。
该研究是一项多中心的、安慰剂为对照的随机双盲试验,将有≥1条SVG的冠状动脉搭桥术后患者随机分至替格瑞洛组或安慰剂组,两组患者均同时附有80或100mg的阿司匹林。主要评估指标是1年内的SVG阻塞率,次要指标为1年内SVG失败,包括SVG阻塞、SVG血运重建、SVG所在心肌区域引起的心肌梗塞或猝死。
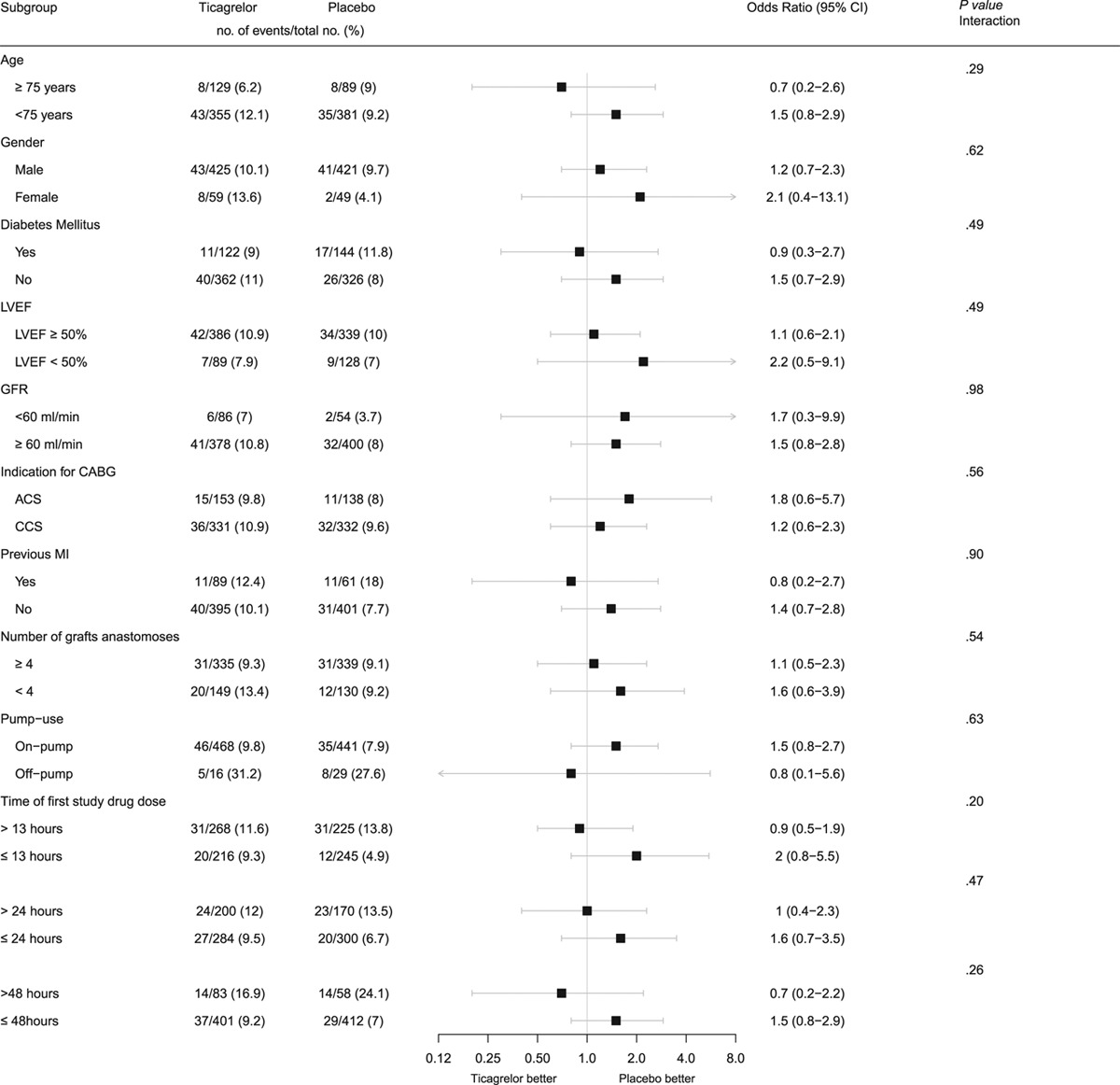
主要预后的亚组分析
共499位受试者,平均67.9±8.3岁,87.1%的男性,31.3%的患者进行CABG的指征为急性冠状动脉综合征,其中95.2%的采用了体外循环。替格瑞洛组和安慰剂组分别有220位和223位患者可进行主要指标评估,两组的SVG阻塞率分别为10.5%和9.1%,优势比 1.29。替格瑞洛组和安慰剂组分别还发生了35例(14.2%)和29例(11.6%)SVG失败,优势比 1.22。
总之,在该随机对照研究中,在标准阿司匹林疗法中加入替格瑞洛并不能降低CABG术后1年内的SVG阻塞率。
原始出处:
Laura M. Willemsen, et al. Effect of Adding Ticagrelor to Standard Aspirin on Saphenous Vein Graft Patency in Patients Undergoing Coronary Artery Bypass Grafting (POPular CABG). Circulation. 2020;142:1799–1807
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#搭桥#
100
#阻塞#
79
#冠脉搭桥术#
75
了解最新资讯
132
#搭桥术#
76
#冠脉搭桥#
111
学习学习
137
感谢分享
136