Nature子刊:天然植物岩蔷薇有望治疗艾滋病毒
2016-02-05 MedSci MedSci原创
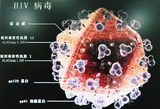
在一项新的研究中,来自德国亥姆霍兹慕尼黑中心的研究人员发现药用植物白瑞木(Cistus incanus,也译作灰白岩蔷薇)的提取物阻止人免疫缺陷病毒(HIV)感染细胞。这种提取物中的抗病毒活性成分抑制HIV病毒蛋白停泊到细胞上。这种提取物中的抗病毒成分也具有抗埃博拉病毒和马尔堡病毒的作用。相关研究结果于2016年2月2日在线发表在Scientific Reports期刊上,论文标题为“Potent
在一项新的研究中,来自德国亥姆霍兹慕尼黑中心的研究人员发现药用植物白瑞木(Cistus incanus,也译作灰白岩蔷薇)的提取物阻止人免疫缺陷病毒(HIV)感染细胞。这种提取物中的抗病毒活性成分抑制HIV病毒蛋白停泊到细胞上。这种提取物中的抗病毒成分也具有抗埃博拉病毒和马尔堡病毒的作用。相关研究结果于2016年2月2日在线发表在Scientific Reports期刊上,论文标题为“Potent in vitro antiviral activity of Cistus incanus extract against HIV and Filoviruses targets viral envelope proteins”。
病毒感染是全世界人类死亡第十大原因之一,也代表着一个巨大的全球健康挑战。对它们的控制需要持续地开发新的强效抗病毒药物/治疗方案。尽管在治疗HIV/AIDS时有众多药物可供选择,但是还需要开发新的药物来阻止耐药性病毒变异体出现。再者,在急性病毒传染病爆发期间,也需要开发新的抗病毒药物来快速治疗由诸如马尔堡病毒和埃博拉病毒之类的病毒导致的急性感染。在这项新的研究中,来自亥姆霍兹慕尼黑中心病毒研究所的Ruth Brack-Werner教授、Stephanie Rebensburg博士及其团队证实药用植物白瑞木提取物攻击HIV和埃博拉病毒颗粒,并阻止它们在体外培养的细胞中增殖。
HIV:广谱性,没有耐药性
Brack-Werner团队发现白瑞木提取物能够抵抗各种临床HIV-1和HIV-2分离株,这其中还包括一种几乎对大多数市场上销售的药物产生耐药性的病毒分离株。Brack-Werner解释道,“白瑞木提取物的抗病毒成分靶向作用于HIV传染性颗粒表面上的病毒膜蛋白,并阻止它们接触宿主细胞。”在长期使用(24周)白瑞木提取物期间,并没有检测到耐药性毒株,这意味着白瑞木提取物在攻击病毒的同时不会产生过耐药性。这项研究表明来自诸如白瑞木之类的植物或诸如狭花天竺葵(Pelargonium sidoides)之类的其他植物的商用草本植物提取物有望被用来开发得到科学验证的抗病毒植物治疗药物。Brack-Werner说,“鉴于白瑞木提取物的抗病毒活性与所有得到临床批准使用的药物存在不同,源自白瑞木的产品可能成为当前也已建立的药物治疗方案的一个重要补充。”
编者注:关于狭花天竺葵提取物阻止HIV病毒感染的报道,可参见MedSci新闻报道:PLoS ONE:天竺葵属老鹳草提取物具有对抗艾滋病HIV-1病毒的作用。
白瑞木提取物也靶向攻击病毒颗粒上的埃博拉病毒蛋白和马尔堡病毒蛋白
白瑞木提取物不仅阻断不同的HIV分离株,而且阻断携带马尔堡病毒蛋白和埃博拉病毒膜蛋白的病毒颗粒。对该提取物中的抗病毒成分进行的分析揭示出多种抗病毒组分的存在,其中这些组分可能组合在一起发挥作用。这些结果强有力地表明白瑞木提取物对多种主要的人病毒病原体具有广谱的抗病毒活性,包括之前报道的抗流感病毒活性。
白瑞木提取物对全球控制致命病毒感染的潜在应用
进一步开发这些植物提取物可能以多种方式加快对病毒感染的全球治疗和控制。因此,这些植物提取物可能是开发强效的抗病毒感染草药试剂的起始材料。另一项应用可能是将它们开发为阻断诸如HIV之类的病毒传播的乳油或凝胶(即杀微生物剂)。最后,这些植物提取物含有很多大有希望的天然抗病毒试剂,有望从中发现新的抗病毒分子。
Brack-Werner实验室的未来研究工作将重点研究这些植物来源产品在人体内的抗病毒潜力以及它们的抗病毒活性成分进行的详细分析。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











希望有用.尽快进去临床试验吧.
82
#Nat#
48
#植物#
53
实践中,发展~
154
看看能诺奖?
148
祈祷吧
203
哦
111
牛
89
重要
100
希望能成功。
70