cell综述:阿尔茨海默病30年来的研究进展
2012-04-16 陈蓉 生物通
来自加州大学旧金山分校,Gladstone神经疾病研究所的Lennart Mucke和黄亚东教授发表了题为“Alzheimer Mechanisms and Therapeutic Strategies”的文章,总结概括了过去三十年里,这一疾病的发展,指出这一领域的研究探讨和药物研发,应该多元化发展,来解析阿尔茨海默病这一多因素影响
这篇Cell综述【综述全文下载地址Cell.2012-03-16;148(6):1204-22.】指出,对于阿尔茨海默病这一早已被发现的疾病,目前仍然没有有效的方法,能预防,治疗或者逆转阿尔茨海默病患者症状,但是在过去三十年中,这一领域也取得了不少突破性性的进展。
遗传学研究证明这种疾病是由多种因素引发的,跨学科的技术方法——复合生物化学,分子和细胞生物学,以及转基因模型都揭示了其中的分子机制。化学,放射学科,以及系统生物学也开始逐步用于这一疾病的治疗,提供了有效的生物标记,并且个性化医疗方法的出现也有望改变药物研发和临床实验的面貌。
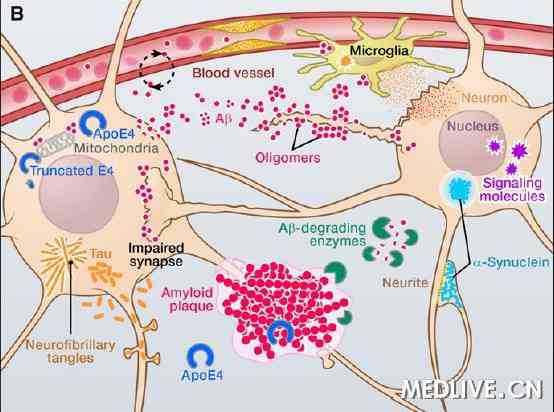
作者还指出,由于阿尔茨海默病是一种受到多因素影响的疾病,这一领域的研究探讨和药物研发,应该多元化发展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
相关资讯
Neurology:阿尔茨海默病新标志物VILIP-1可能预测心智能力下降
3月6日,《神经病学》(Neurology)杂志上的一项研究论文称,圣路易斯华盛顿大学医学院的研究人员发现阿尔茨海默病的一个新标志物可预测患者确诊后的记忆力及其他心智能力下降的速度。 在60例早期阿尔茨海默病患者中,脊髓液中较高水平的标志物(视锥蛋白样蛋白1(VILIP-1))与随后数年较快的心智能力下降相关。 科学家需要在更大规模的研究中证实该结果,但新数据表明, VILIP-1可能成为预测
Arch Neurol:抗氧化治疗或对阿尔茨海默病无效
3月19日,国际杂志Archives of Neurology在线刊登的一篇研究表明,联合抗氧化治疗并不能改变阿尔茨海默病(AD)患者脑脊液中病理相关标志物水平。 研究显示在对轻中度AD患者使用维生素E、维生素C 和α硫辛酸(ALA)联合抗氧化治疗16周后,其淀粉样蛋白和tau蛋白相关的脑脊液标志物并没有改变,MMSE量表结果显示认知功能呈恶化趋势,但脑脊液中F2-isoprostane(脑
FDA批准阿尔茨海默病检测新法
4月6日,美国食品与药物管理局(FDA)批准用一种放射性化合物评估阿尔茨海默病患者的认知损伤。这种名为Amyvid的药物能够与淀粉体斑块结合在一起,在进行正电子发射层析(PET)扫描之前,Amyvid使得医生能够看清淀粉体是否已经开始在大脑中积聚。 图片来源:美国国立卫生研究院 &n
神经退行性疾病:小胶质预备,go...
许多研究表明,小胶质启动加剧了几种神经退行性疾病的进程,例如阿尔茨海默氏症和朊病毒疾病。然而在启动过程的开始背后的分子路径依然没有得到很好的了解,但是一项新的研究显示,补体系统的调节失常很可能与此有关。 补体调节蛋白CRRY是啮齿动物中的“替代路径”的一种重
J Neurosci:抗癌药或能用于早期阿尔茨海默病的治疗
根据一项新的研究证实,一种已经进步II期临床试验实验的、治疗癌症的化合物能在阿尔茨海默氏症的动物模型减慢神经损伤和改善大脑功能。3月13,Journal of Neuroscience杂志刊登的一则研究表明:埃博霉素D(EpoD)在阿尔茨海默氏病的小鼠模型(AD)中能有效地防止神经损伤、改善认知表现。这些结果接揭示将来或许该药物能用于早期AD患
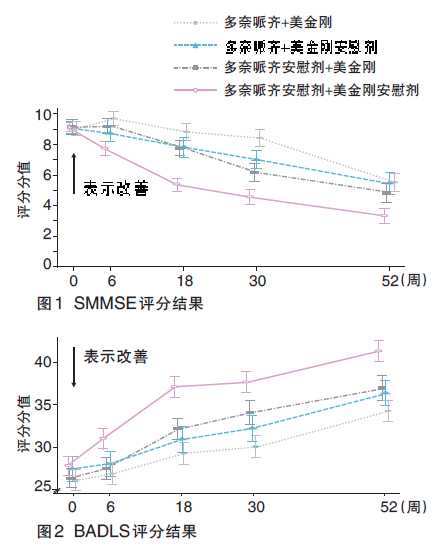
NEJM研究启示:治疗中重度AD,多奈哌齐是理想选择
流行病学资料显示,在65岁及以上的老年人中,阿尔茨海默病(AD)患病率为4.4%,且年龄每增加5岁,患病率翻一番。随着世界人口日趋老龄化,AD已成为当前老年医学面临的最严峻问题之一。据估计,2010年全球约有3560万AD患者,2030年将达6570万。在我国,约有600万AD患者,如果不能有效控制,2030年将达1500万。 >&










#Cell#
70
#CEL#
55
#阿尔茨海#
83
#阿尔茨#
84
#研究进展#
64
#阿尔茨海默#
59