PLOS ONE:科学家开发出新技术有效预测2型糖尿病风险!
2017-08-29 枫丹白露 来宝网
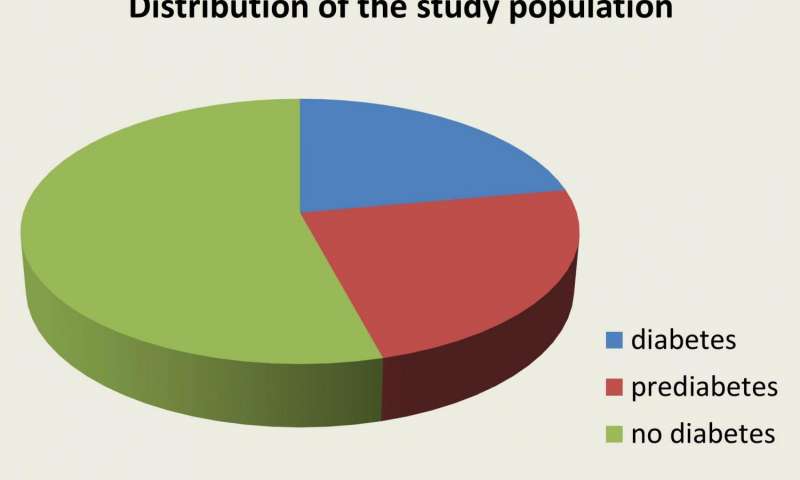
格拉斯哥大学的研究人员已经宣布了一种新的基于技术的方法,可以更准确地识别2型糖尿病高危人群。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#2型糖尿病风险#
55
#Plos one#
69
#新技术#
60
技术在发展
82
学习一下很不错
82