BMC Cancer:随访长达10年的前瞻性研究证实女性非转移性乳腺癌患者越年轻预后越差
2022-01-09 yd2015 MedSci原创
该前瞻性研究证实年轻(<40岁)是非转移性乳腺癌患者的不良预后因素。
既往研究表明年轻(<40岁)是女性乳腺癌患者不良结局的独立危险因素。近期,BMC Cancer杂志上发表了一项随访长达10年的前瞻性研究结果,评估≥40岁和<40岁女性非转移乳腺癌患者的生存差异,还探索影响生存的肿瘤特征、分子标志物和免疫组合标志物等因素对生存的影响。

在2011年7月至2014年5月间,共有119名患者被招募入本研究。所有患者的中位年龄为44岁(2776岁)。73例(62%)患者年龄≥40岁,中位年龄为51(41-76)岁。46例(39%)患者<40岁,中位年龄36.5岁(27-39岁)。
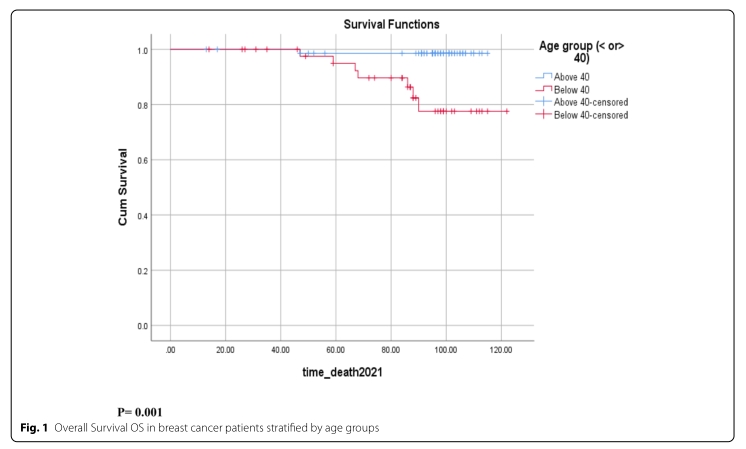
中位随访时间为96个月,范围为13 - 122个月。≥40岁患者的10年OS率为98.6%,<40岁患者的10年OS率为77.6% (p = 0.001)。
≥40岁患者的10年DFS率为90%,<40岁患者的10年DFS率为70.4% (p = 0.004)。

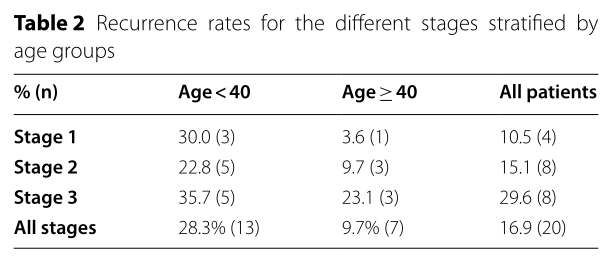
I期患者中,≥40岁和<40岁患者的复发率分别为30%和3.6%(p=0.016);II期患者中分别为22.8%和9.7%(p=0.116);III期分别为35.7%和23.1%(p=0.402)
综上,该前瞻性研究证实年轻(<40岁)是非转移性乳腺癌患者的不良预后因素。
原始出处:
Bouferraa Y, Haibe Y, Chedid A, Jabra E, Charafeddine M, Temraz S, Mukherji D, El Saghir N, Shamseddine A. The impact of young age (< 40 years) on the outcome of a cohort of patients with primary non-metastatic breast cancer: analysis of 10-year survival of a prospective study. BMC Cancer. 2022 Jan 3;22(1):27. doi: 10.1186/s12885-021-09100-z. PMID: 34980002; PMCID: PMC8722326.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#非转移#
80
#BMC#
55
#前瞻性#
0
#非转移性#
74
#前瞻性研究#
68
学习学习
54
#转移性#
71
#乳腺癌患者#
67
I期患者中,≥40岁和<40岁患者的复发率分别为30%和3.6%(p=0.016);II期患者中分别为22.8%和9.7%(p=0.116);III期分别为35.7%和23.1%(p=0.402) 这里年龄写反了吧,应该是 I期患者中,<40岁和 ≥40岁患者的复发率分别为30%和3.6%(p=0.016);II期患者中分别为22.8%和9.7%(p=0.116);III期分别为35.7%和23.1%(p=0.402)
73