Cancer Cell:胸腺基质淋巴生成素(TSLP)或抵御皮肤癌
2012-12-10 T.Shen 生物谷
近日,来自华盛顿大学医学院等处的研究者研究发现,一种和哮喘、过敏相关的分子可以使得小鼠对皮肤癌产生抗性,相关研究成果刊登于近日的国际杂志Cancer Cell上。 这种分子称为TSLP(thymic stromal lymphopoietin,胸腺基质淋巴生成素),其由损伤的皮肤产生,可以激活免疫系统。长期的低水平TSL

近日,来自华盛顿大学医学院等处的研究者研究发现,一种和哮喘、过敏相关的分子可以使得小鼠对皮肤癌产生抗性,相关研究成果刊登于近日的国际杂志Cancer Cell上。
这种分子称为TSLP(thymic stromal lymphopoietin,胸腺基质淋巴生成素),其由损伤的皮肤产生,可以激活免疫系统。长期的低水平TSLP可以使得免疫系统对于正常无害环境过敏,就会导致皮疹以及常见的哮喘、过敏。
研究者在文章中检测到,可以对皮肤肿瘤有抵抗能力的小鼠,其血液中的TSLP水平是正常小鼠的1000倍以上。而且皮肤中TSLP的水平也非常高。在另一项发表在Cancer Cell上的研究中,研究者也揭示了RSLP可以抑制小鼠皮肤癌的发生。
对于Kopan研究团队来说,他们调查了皮肤中缺少特定信号蛋白的小鼠,这种蛋白名为Notch,其对于形成机体组织,如皮肤组织非常重要。Kopan表示,是否TSLP可以保护小鼠免于皮肤癌?因此他们检测了用于治疗银屑病的药物-卡泊三醇对小鼠的作用,其可以促使皮肤产生TSLP。研究者发现,对正常皮肤用卡泊三醇作用,健康小鼠就会保护自身抵御皮肤癌。
在卡泊三醇的临床试验中,研究者并不能完全确定保护效应产生是否是由于产生了TSLP,未来研究中,研究者希望通过深入研究揭示TSLP是否对其它类型的癌症也有类似的抑制效应。
与皮肤癌相关的拓展阅读:
- Cancer Cell:胸腺基质淋巴生成素或抵御皮肤癌
- JID:蛋白Wnt1抑制皮肤癌转移
- NEJM:从钙调神经磷酸酶抑制剂换为西罗莫司降低肾移植病人患新皮肤癌
- 专家视点:重拾皮肤癌的放射治疗
- PNAS:美研究人员发明纳米级护肤乳液 或可预防皮肤癌 更多信息请点击:有关皮肤癌更多资讯
编译自:Mice at Risk of Asthma, Allergies Can Fight Off Skin Cancer

doi:10.1016/j.ccr.2012.08.016
PMC:
PMID:
Loss of Cutaneous TSLP-Dependent Immune Responses Skews the Balance of Inflammation from Tumor Protective to Tumor Promoting
Matteo Di Piazza, Craig S. Nowell, Ute Koch, André-Dante Durham, Freddy Radtke
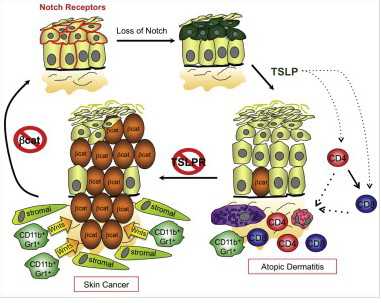
Inflammation can promote or inhibit cancer progression. In this study we have addressed the role of the proinflammatory cytokine thymic stromal lymphopoietin (TSLP) during skin carcinogenesis. Using conditional loss- and gain-of-function mouse models for Notch and Wnt signaling, respectively, we demonstrate that TSLP-mediated inflammation protects against cutaneous carcinogenesis by acting directly on CD4 and CD8 T cells. Genetic ablation of TSLP receptor (TSLPR) perturbs T-cell-mediated protection and results in the accumulation of CD11b+Gr1+ myeloid cells. These promote tumor growth by secreting Wnt ligands and augmenting β-catenin signaling in the neighboring epithelium. Epithelial specific ablation of β-catenin prevents both carcinogenesis and the accumulation of CD11b+Gr1+ myeloid cells, suggesting tumor cells initiate a feed-forward loop that induces protumorigenic inflammation.

doi:10.1016/j.ccr.2012.08.017
PMC:
PMID:
Elevated Epidermal Thymic Stromal Lymphopoietin Levels Establish an Antitumor Environment in the Skin
Shadmehr Demehri, Ahu Turkoz, Sindhu Manivasagam, Laura J. Yockey, Mustafa Turkoz, Raphael Kopan
Thymic Stromal Lymphopoietin (TSLP), a cytokine implicated in induction of T helper 2 (Th2)-mediated allergic inflammation, has recently been shown to stimulate solid tumor growth and metastasis. Conversely, studying mice with clonal loss of Notch signaling in their skin revealed that high levels of TSLP released by barrier-defective skin caused a severe inflammation, resulting in gradual elimination of Notch-deficient epidermal clones and resistance to skin tumorigenesis. We found CD4+ T cells to be both required and sufficient to mediate these effects of TSLP. Importantly, TSLP overexpression in wild-type skin also caused resistance to tumorigenesis, confirming that TSLP functions as a tumor suppressor in the skin.
(责任编辑:yan.mao)
分享到:本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
66
#胸腺#
91
#CEL#
0
#cancer cell#
52
#基质#
61
#Cell#
76