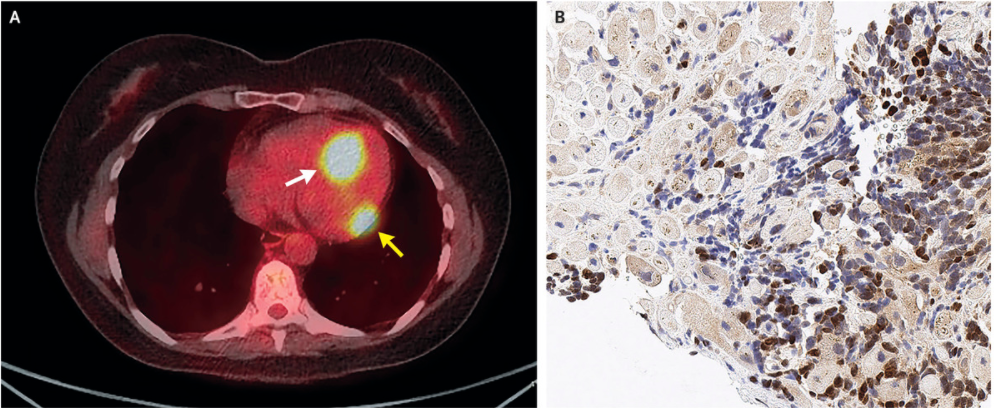
Cell Rep:黑素脱失患者来源多能性干细胞的自体移植治疗 -色素恢复与皮肤功能重建取得重大突破
2019-04-10 不详 细胞
近日,Cell Reports公布了一项皮肤再生医学研究领域的重要进展:《患者iPS细胞来源的诱导黑素细胞在自体移植治疗中的潜能》(Therapeutic potential of patient iPSC-derived iMelanocytes in autologoustransplantation)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#色素#
64
#Cell#
54
#CEL#
74
#自体移植#
74