Cell Res:阎锡蕴团队在动脉粥样硬化机制研究中获进展
2017-04-24 佚名 生物物理研究所
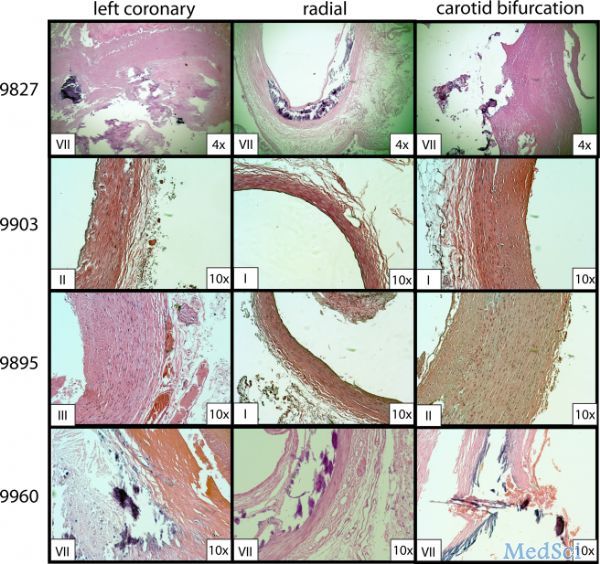
动脉粥样硬化是冠心病及缺血性脑血管病发生的主要原因。随着人们生活方式的改变,尤其是高脂饮食,动脉粥样硬化的发病率显着上升,由此而导致的死亡率也逐年增加。如何预防和治疗动脉粥样硬化是一个全民关注的健康难题。众所周知,动脉粥样硬化的主要病理特征是大中动脉血管内膜下斑块形成,其中易损斑块容易破裂出血,与心脑血管事件的发生密切相关。易损斑块的形成有以下两个重要因素:一,巨噬细胞泡沫化,即斑块中的巨噬细胞大
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#机制研究#
74
#粥样硬化#
58
#CEL#
81
#Cell#
60
学习了,谢谢分享
80