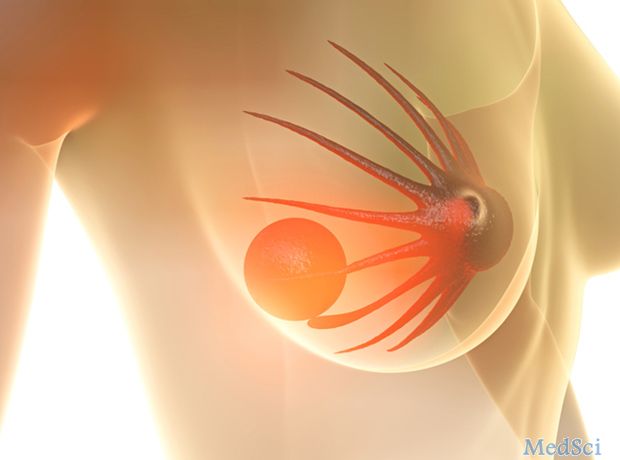
诺华kisqali表明可显著延长绝经前乳腺癌患者的无进展生存期
2017-12-07 MedSci MedSci原创
诺华公布了III期临床数据,显示与单独进行内分泌治疗的乳腺癌患者相比,与内分泌疗法合用Kisqali可显著延长无进展生存期(PFS)。在III期MONALEESA-7试验中,Kisqali联合他莫昔芬或芳香化酶抑制剂加戈舍瑞林治疗绝经前或围绝经期女性激素受体阳性,人类表皮生长因子受体2阴性(HR + / HER2-)晚期或转移性乳腺癌的PFS中位数为23.8个月,而他莫昔芬或芳香化酶抑制剂加上戈舍
诺华公布了III期临床数据,显示与单独进行内分泌治疗的乳腺癌患者相比,与内分泌疗法合用Kisqali可显著延长无进展生存期(PFS)。在III期MONALEESA-7试验中,Kisqali联合他莫昔芬或芳香化酶抑制剂加戈舍瑞林治疗绝经前或围绝经期女性激素受体阳性,人类表皮生长因子受体2阴性(HR + / HER2-)晚期或转移性乳腺癌的PFS中位数为23.8个月,而他莫昔芬或芳香化酶抑制剂加上戈舍瑞林为13.0个月。该药物巨头指出,在接受Kisqali联合疗法治疗的绝经前女性中,早在八周的时候就有了对内分泌治疗的反应。"MONALEESA-7数据的优势是令人印象深刻的,如果ribociclib被批准作为该患者群体的治疗方案,并给予该药物的内分泌治疗选择更大的灵活性,将给肿瘤学家提供一个重要的选择。" 德州大学安德森癌症中心乳腺肿瘤内科主任Debu Tripathy表示。"在乳腺癌诊断时绝经前的妇女往往更具侵袭性,预后较差,伴随着独特的需求和经验,因此确定哪种治疗方法最有效而且耐受性好是至关重要的。MONALEESA-7试验还评估了Kisqali联合他莫昔芬和一种芳香化酶抑制剂PFS为2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#绝经前#
46
#Kisqali#
69
#绝经#
44
#诺华#
54
#生存期#
44
#无进展生存期#
67
#乳腺癌患者#
32