肱骨远端骨折:如何固定才能保证恢复如初?
2018-09-30 沈惠良 姜保国 老年骨质疏松骨折
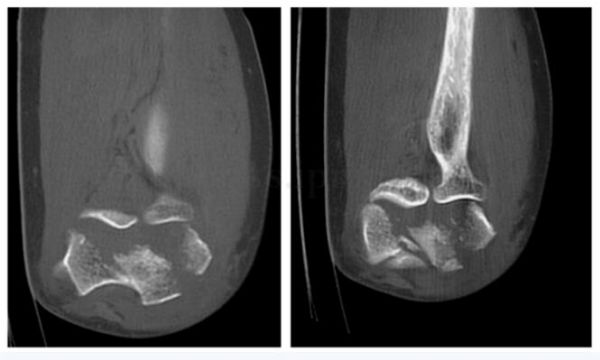
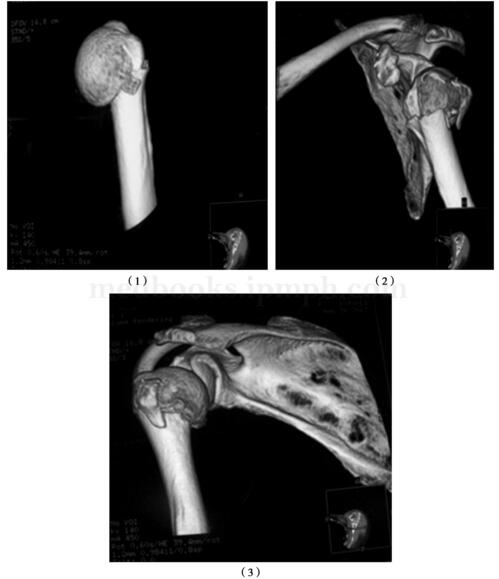
54岁女性,不慎摔倒,右肘部着地,当即感右肘部疼痛剧烈,伴活动受限。X 线片提示:右肱骨远端骨折。肱骨远端骨折属于复杂的关节内骨折之一,近年临床上提倡哪种治疗方法?



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肱骨远端#
86
#肱骨#
83
学习了长知识
92
学习了长知识
97
学习了长知识
94
学习了长知识
102
学习了长知识
93
学习了长知识
60
学习了长知识
61
学习了长知识
64