性福音!艾伯维妇科药物Elagolix治疗子宫内膜异位症III期项目大获成功
2016-02-19 佚名 生物谷
艾伯维(AbbVie)与合作伙伴Neurocrine Biosciences近日公布了妇科药物Elagolix治疗子宫内膜异位症(endometriosis,EMs)的2个关键III期研究中的第二个临床研究(M12-671)的积极顶线数据。这些研究旨在评估Elagolix治疗绝经前女性子宫内膜异位症的疗效和安全性。 此次公布的M12-671研究结果表明,经过6个月的连续治疗,
艾伯维(AbbVie)与合作伙伴Neurocrine Biosciences近日公布了妇科药物Elagolix治疗子宫内膜异位症(endometriosis,EMs)的2个关键III期研究中的第二个临床研究(M12-671)的积极顶线数据。这些研究旨在评估Elagolix治疗绝经前女性子宫内膜异位症的疗效和安全性。
此次公布的M12-671研究结果表明,经过6个月的连续治疗,Elagolix 150mg QD(150mg/每天一次)和200mg BID(200mg/每天2次)2个剂量组均达到了研究的共同主要终点:在研究的3个月和6个月,Elagolix均有效减少了由子宫内膜异位症引起的痛经(DYS)和非经期盆腔疼痛(NMPP)。该项研究中,实现共同主要终点的应答者(responder)比例与首个关键III期研究(M12-665)的结果保持一致,数据如下表所示。这2个关键III期研究(M12-665,M12-671)的详细数据将提交至2016年召开的医学会议。艾伯维已计划在2017年提交Elagolix治疗子宫内膜异位症的新药申请(NDA)。
艾伯维与Neurocrine于2010年签署6亿美元协议合作开发Elagolix。之前,Evaluate Pharma发布《2016年上市的十大潜力药品》榜单,其中Elagolix位居第10位,该药2020年的年销售额预计将达到9亿美元。
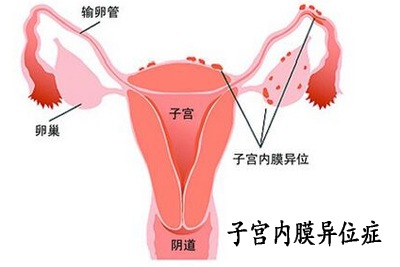
子宫内膜异位症(Ems)是育龄期女性较为常见的临床良性疾病,其发生率达10.0%,且呈明显之上升趋势,该病以痛经、盆腔疼痛及不孕为主要特征,严重影响女性的生殖健康和生活质量。

据估计,在全球范围内,多达1.76亿女性受子宫内膜异位症困扰,而目前该病的临床管理迫切需要更多的治疗选择,因此该领域存在着巨大的未获满足的医疗需求。为满足这一需求,艾伯维针对子宫内膜异位症开展了全球最大的前瞻性临床项目。截至目前为止,该项目的结果非常令人满意。艾伯维表示,将继续探索Elagolix作为一种潜在新药,用于治疗子宫内膜异位症最常见的症状,包括经期疼痛(痛经)以及伴随整个月经周期的慢性盆腔疼痛。
安全性方面,Elagolix在该研究中与首个关键III期研究及既往研究一致,与治疗相关的最常见不良事件(TEAE)包括潮热、头痛、恶心。根据Elagolix作用机制预期出现的不良事件(AE),例如潮热、雌激素过低相关TEAEs及骨密度(BMD)变化呈剂量依赖。总体停药率在各个治疗组相似,安慰剂组、Elagolix 150mg QD组、200mg BID组停药率分别为25.3%、21.2%、19.7%,TEAE导致的停药率分别为6.1%、4.4%、10.0%。6个月时腰椎骨密度(LS)从基线的平均变化如下表所示。Elagolix 150mg QD的BMD数据与先前的II期研究结果一致,Elagolix 200mg BID的BMD数据呈剂量依赖性效应。

关于子宫内膜异位症(EMs):
子宫内膜异位症(endometriosis,EMs)是指内膜细胞种植在不正常的位置而形成的一种女性常见妇科疾病。内膜细胞本该生长在子宫腔内,但由于子宫腔通过输卵管与卵巢、盆腔相通,因此使得内膜细胞可经由输卵管进入卵巢、盆腔及子宫邻近区域异位生长。
目前,尚无任何药物能够治愈子宫内膜异位症。在临床上,目前该病通过口服避孕药、非甾体类抗炎药、阿片类药物、促性腺激素释放激素(GnRH)拮抗剂进行管理。当这些药物治疗失败后,常常采用手术干预(例如,剖腹手术或腹腔镜手术),但这些措施仍然无法治愈子宫内膜异位症。痛经是子宫内膜异位症最典型的症状,此外,患者常伴有不孕不育。
关于Elagolix:
Elagolix是一种口服促性腺激素释放激素(GnRH)拮抗剂,通过抑制脑垂体促性腺释放激素受体,最终降低血循环中性腺激素水平。目前,艾伯维正在调查Elagolix治疗一些由性激素介导的疾病,如子宫肌瘤、子宫内膜异位症。到目前为止,Elagolix的临床试验超过40个,涉及患者总数超过3000例。另外,Elagolix治疗子宫肌瘤的III期临床试验也正在进行中。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#III#
51
#Elagolix#
62
#内膜#
69
#子宫内膜异位#
67
#性福#
67
#艾伯维#
68
#III期#
66
赞
117
赞
160