JAMA Neurology: COMT抑制剂对帕金森左旋多巴疗法辅助效果不佳
2022-01-09 影像小生 MedSci原创
与MAO-B抑制剂或多巴胺激动剂作为左旋多巴治疗不可控PD患者的辅助治疗相比,COMT抑制剂的患者分级生活质量更差。
在左旋多巴治疗中加入多巴胺再摄取抑制剂(DRI)(单胺氧化酶B型(MAO-B)抑制剂或邻苯二酚- o -甲基转移酶(COMT)抑制剂)是否比添加多巴胺激动剂更有效,如果DRI更有效,在左旋多巴治疗无法控制的帕金森病运动并发症患者中,哪种DRI级(MAO-B或COMT)更有利于改善患者的生活质量。
许多帕金森病患者出现左旋多巴剂量调整无法控制的运动并发症。在这些患者中,尚不清楚哪种药物作为辅助治疗更有效。
Richard Gray等比较了左旋多巴治疗中添加多巴胺激动剂和多巴胺再摄取抑制剂(DRI)对PD运动并发症患者的长期生活质量的影响。

这项实用的半阶乘随机临床试验从2001年2月23日至2009年12月15日期间的64个神经病学和老年病学诊所(英国62个,捷克1个,俄罗斯1个)中招募。共有500名发生了不可控运动并发症且没有痴呆的特发性PD患者被随机分配在1:1:1的组中。
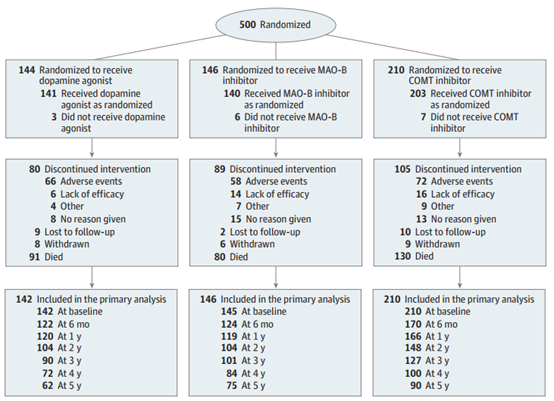
干预因素为开放标签多巴胺激动剂,MAO-B抑制剂,或COMT抑制剂。主要评估指标为39项帕金森病问卷(PDQ-39)活动域和成本-效果评分。研究开始前、随机分组后6个月和12个月以及之后每年评估一次结果。
500名参与者的平均年龄(SD)为73.0岁(8.2岁);314名(62.8%)是男性。
在中位4.5年(范围0-13.3年)的随访中,多巴胺激动剂组参与者的平均PDQ-39活动评分为2.4分(95% CI, 1.3 - 6.0分),优于联合MAO-B和COMT组;然而,这种差异不显著(P= 0.20)。
关于DRIs, MAO-B组参与者的平均PDQ-39活动得分为4.2分(95% CI, 0.4-7.9分;P=0.03)优于COMT组;
EuroQol 5维3-level (EQ-5D-3L)效用评分为0.05分(95% CI, 0.003-0.09分;P=0.04)优于COMT组。
治疗组间预后指标的估计平均差异
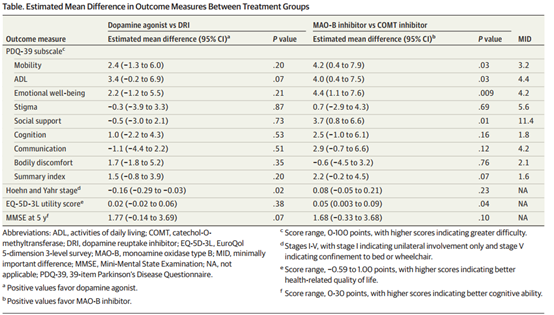
PDQ-39汇总指数无显著改善(平均差异2.2分;95% CI, 0.2 ~ 4.5分;P=.07),同时痴呆发生率 (比率[RR], 0.70;95%置信区间,0.47 - -1.03;P = 0.07)和死亡率(RR, 0.76;95%置信区间,0.56 - -1.03;P = . 07) 无显著降低。多巴胺激动剂与单抗MAO-B抑制剂比较结果相似。
在左旋多巴治疗无法控制运动并发症的PD患者中,COMT抑制剂作为辅助治疗时,患者的生活质量低于MAO-B抑制剂或多巴胺激动剂。MAO-B抑制剂产生了等效的疾病控制,这表明这些药物可能没有充分用于辅助治疗。
原文出处
Gray R, Patel S, Ives N, et al. Long-term Effectiveness of Adjuvant Treatment With Catechol-O-Methyltransferase or Monoamine Oxidase B Inhibitors Compared With Dopamine Agonists Among Patients With Parkinson Disease Uncontrolled by Levodopa Therapy: The PD MED Randomized Clinical Trial. JAMA Neurol. Published online December 28, 2021. doi:10.1001/jamaneurol.2021.4736
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
78
#Neurol#
92
#COMT#
111
#左旋多巴#
100