ISC 2015:脱水与卒中病情加重具有相关性
2015-02-16 高晓方 译 医学论坛网
国际卒中大会(ISC 2015)公布的一项研究表明,与脱水患者相比,卒中发生时水液平衡良好的患者更有可能转归更佳。 两组患者NIHSS从入院至出院的变化 此项研究共纳入168例缺血性卒中患者,并利用BUN/肌酐比和尿比重评估了患者的水液平衡状况。肾衰患者被排除在外。基于NIHSS评分追踪患者每日卒中严重度,并利用MRI扫描计算卒中所致的脑损伤体积。 结果显示,42%的
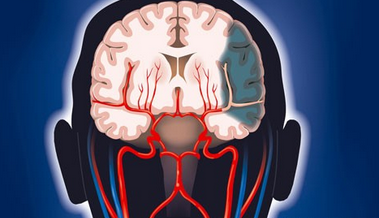
国际卒中大会(ISC 2015)公布的一项研究表明,与脱水患者相比,卒中发生时水液平衡良好的患者更有可能转归更佳。

两组患者NIHSS从入院至出院的变化
此项研究共纳入168例缺血性卒中患者,并利用BUN/肌酐比和尿比重评估了患者的水液平衡状况。肾衰患者被排除在外。基于NIHSS评分追踪患者每日卒中严重度,并利用MRI扫描计算卒中所致的脑损伤体积。
结果显示,42%的脱水患者卒中情况恶化或维持原状,水合良好患者则仅为17%。脱水卒中患者病情恶化风险约为水液平衡良好患者的4倍。
对年龄、初始NIHSS评分、病变体积和血糖进行校正之后,脱水仍对患者病情具有负面影响。卒中时发生时水液平衡良好与卒中转归较好具有相关性。
Abstract T MP86: A Prospective Study of the Effect of Dehydration on Stroke Severity and Short Term Outcome
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










有意思
123
又学习了
132
#相关性#
66
#病情#
65
#病情加重#
64
#ISC#
46
以阅
150