杨紫出荨麻疹满脸红痕 这些皮肤病会“秋后算账”
2016-10-09 责编:朱晓慧、陈康清 人民网-健康时报
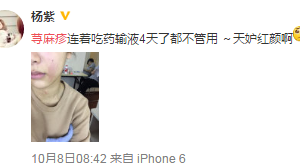
10月8日上午,杨紫在微博晒出一张半脸照,称“荨麻疹连着吃药输液4天了都不管用”。虽然只露出半脸,但依旧看出脸色略微苍白,气色不佳,从脸到脖子一块块红色皮疹相当明显。一入秋,皮肤问题就一箩筐堆来,对于荨麻疹患者,日常中要特别注意这些习惯,否则会导致久治不愈。过度搔抓瘙痒是皮肤病最常见的临床症状,皮肤痒了就会产生搔抓的欲望,一点儿不搔抓是不现实的,但是过度搔抓会加重皮肤病。许多患者为图一时痛快,
10月8日上午,杨紫在微博晒出一张半脸照,称“荨麻疹连着吃药输液4天了都不管用”。虽然只露出半脸,但依旧看出脸色略微苍白,气色不佳,从脸到脖子一块块红色皮疹相当明显。一入秋,皮肤问题就一箩筐堆来,对于荨麻疹患者,日常中要特别注意这些习惯,否则会导致久治不愈。

过度搔抓
瘙痒是皮肤病最常见的临床症状,皮肤痒了就会产生搔抓的欲望,一点儿不搔抓是不现实的,但是过度搔抓会加重皮肤病。许多患者为图一时痛快,用力搔抓皮肤瘙痒处,直抓到皮肤出血为止,结果越抓越痒,越痒越抓,形成恶性循环。
其实,过度搔抓可导致许多皮肤病加重,比如可使神经性皮炎的病变皮肤逐渐粗糙、肥厚;可使急性湿疹进一步扩散,加重渗出,所以,皮肤病患者在治疗的同时,一定要管住自己的手,尽可能避免搔抓,瘙痒剧烈时可及时服药或涂药止痒。
热水烫洗
许多患者为图一时之快用热水烫洗皮疹,虽然这样能解一时之痒,但过后会加剧瘙痒,尤其是急性湿疹等皮炎,热水烫洗能使毛细血管通透性增加,促进过敏物质大量释放,导致渗出和糜烂加重,使病情恶化。所以,即使是中药熏洗和目前流行的桑拿浴,对于急性湿疹和急性皮炎患者也是不适宜的。
使用碱性洗涤剂
许多皮肤病患者,如手部皲裂性湿疹患者有反复使用碱性肥皂、洗衣粉或洗涤灵洗手的习惯。其实,这些洗涤用品容易导致皮肤更加干燥,使皲裂、瘙痒加重。老年性皮肤瘙痒症用肥皂洗澡可抑制皮脂分泌,使皮肤更干燥,从而加重瘙痒。因此,这类患者可试用含油脂丰富的香皂。
饮食不节
一些人可因食海鲜、狗肉、牛羊肉、鱼、虾、蟹、蚕蛹及各种刺激性食品,如吃辣椒、花椒、大蒜、肉桂、韭菜等,而诱发湿疹,荨麻疹等变态反应性皮肤病,或使其加重。因此,对过敏体质者来说,应避免辛辣刺激之品,饮食宜清淡,可适当吃些水果,补充多种维生素。
滥用药物
可以说,因滥用药物而导致皮肤病加重等现象比比皆是。例如外用皮质类固醇治疗手癣。结果导致皮疹范围越来越广泛。面部脂溢性皮炎长期外用激素,引发顽固难治的激素依赖性皮炎、急性糜烂渗出性湿疹,滥用软膏类制剂,导致皮疹扩散,渗出加重。
所以,治疗皮肤病首先要明确诊断,针对病因,根据皮疹的形态,选择恰当的治疗方法。
专家提醒,有一些皮肤病容易“秋后算账”——
带状疱疹
带状疱疹,是由水痘-带状疱疹病毒引起的,平时潜伏在人体某个神经节上,成年人绝大部分是这种病毒的携带者,当人体免疫力较强时,这种病毒一般不会发作;而当抵抗力下降时,这种病毒就会复制,沿着神经分布下行,从而使皮肤出现红斑、丘疹水疱,并伴有剧烈疼痛。
带状疱疹俗称“蛇丹”、“缠腰龙”或“蜘蛛疮”,好发于春秋季节,成年人多见,尤其是老年人、久病体虚、身体疲劳、癌症、感冒等人群。
该病初期有时会先出现疼痛,容易被误诊为心绞痛、溃疡病、胆道痛或肾绞痛,但疼痛四五天甚至更长时间后会出现皮疹。不少患者对此不了解,以为是脏器出了问题或是皮肤过敏,就看消化内科或自行服用过敏药、擦止痒软膏,很多患者会等到皮肤出现皮疹后才到皮肤科就诊,因而耽误了最佳的治疗期,留下了顽固性神经痛。
由于现代生活节奏快,竞争压力大,使年轻人格外珍惜自己的工作,干起活来常常是废寝忘食;同样,物质生活的不断丰富又使老年人能够打发时光、消遣度日的娱乐也多起来了,玩棋牌、看电视,熬夜的本领也不逊于年轻人。疲惫的身心无疑会增加生病的机会。因此,现在门诊的皮肤病患者中带状疱疹比以前明显增多。
因为感冒发烧时人体抵抗力较低,易诱发该病毒。同时要注意休息,不要熬夜。换季时要注意不要着凉。尤其在秋季,要注意补充水分,可适量服用一些维生素,尤其是维生素C、维生素B和维生素E,并加强日常身体锻炼,以增强抵抗力。
虽然带状疱疹很少引起全身症状或并发症,但因其疼痛较重,严重地影响到人们的日常生活,因此有了皮肤骤起的红色丘疹水疱并有疼痛时,应及时到皮肤病专科医院或正规医院的皮肤科就诊,越早治疗效果越好。
瘙痒症
皮肤瘙痒症是一种自觉皮肤瘙痒而无原发性损害的皮肤病。皮肤瘙痒原因复杂,全身性皮肤瘙痒常见原因为内分泌失调和冬季瘙痒,肝肾疾病、恶性肿瘤及精神性因素也可引起瘙痒,过度清洁皮肤造成皮肤脱脂干燥而产生瘙痒。
常见症状有:1.剧烈瘙痒。可见于全身或局限于肛门、阴囊或女阴部。为阵发性,痒感剧烈,常在夜间加重,影响睡眠。病人常用手抓挠不止。2.继发性皮损。抓挠过度而发生抓痕、血淤,日久可出现湿疹化、苔藓样变及色素沉着。
天气转凉,人体皮脂腺分泌减少,皮肤容易干燥,引起瘙痒。而老年人的皮脂腺分泌功能有所减退,皮肤更干燥。同时,再加上一些外部的刺激,如过多使用肥皂、洗衣粉、洗澡太勤、搓澡太用力等,极易引起瘙痒。
对于患有皮肤瘙痒症,且每逢换季时节病情就较重的患者,建议在换季时做好预防。第一,注意“忌嘴”。对于鱼、虾、酒、辣椒等食物尽量不要食用,以免加重病情;第二,尽量少接触含有化学成分的物品,如洗衣粉等;第三,皮肤痒时,切忌抓挠或用开水烫,可搽一些润肤乳液、服用一些抗过敏药物或养血润燥、祛风止痒的中药;平时少用肥皂洗手,注意护肤。
瘙痒如果反复发作,会影响情绪,使人精神受到不良刺激,造成失眠或睡眠浅表,甚至改变人的性格,易于暴躁不安。因此,瘙痒是有损病人尤其是老人健康的一个大敌。因此,皮肤瘙痒不可忽视,不可不治。
银屑病
银屑病俗称“牛皮癣”,是一种常见的慢性红斑鳞屑性皮肤病。银屑病的临床症状多种多样,比较轻的有寻常型,严重的有脓疱型、红皮病型和关节病型。根据病情的发展,银屑病又分为进行期、静止期和退行期三期。
诱发银屑病的因素很多,但一个重要因素就是季节变化,该病往往冬天加重夏天减轻。天气转凉,病情常常会逐渐加重。同时,由于发病机理目前并不清楚,该病只能控制而不能根治。所以秋季必须做好预防工作,以免银屑病症状加重或复发。
换季时节,银屑病患者一定要注意保暖,上呼吸道感染是该病的重要诱发因素,而秋季早晚温差大,是上呼吸道感染易发季节,所以避免上呼吸道感染很重要,如果病情加重,一定要及时到医院就诊。另外,在好发季节之前,适当服用凉血消斑润肤中药,能够有效避免银屑病复发。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#皮肤病#
69
安利了。
100
以明星切入讲案例很好!
95
赞了
104
继续关注!
98
谢谢分享!
95
谢谢分享,
50
学习啦,
45
#麻疹#
50
了解一下!
44