JCEM:雌激素诱导甲状腺乳头状癌细胞的自噬
2015-04-29 沐晴 译 MedSci原创
甲状腺乳头状癌(PTC)的发生率在性别中的比例是女:男(1:3),关于性别差异的风险因素知之甚少。越来越多的研究认为雌激素在甲状腺肿瘤的发生中起重要作用,但是相关的机制并不清楚。近来有研究发现雌激素受体α(ER-α)可通过刺激活性氧的生成和胞外信号调节激酶诱导PTC的自噬。 研究者分析了ER-α在PTC患者甲状腺组织中的表达。通过化学和基因技术抑制PTC细胞自噬,检测PTC细胞的活力、增殖和
甲状腺乳头状癌(PTC)的发生率在性别中的比例是女:男(1:3),关于性别差异的风险因素知之甚少。越来越多的研究认为雌激素在甲状腺肿瘤的发生中起重要作用,但是相关的机制并不清楚。近来有研究发现雌激素受体α(ER-α)可通过刺激活性氧的生成和胞外信号调节激酶诱导PTC的自噬。
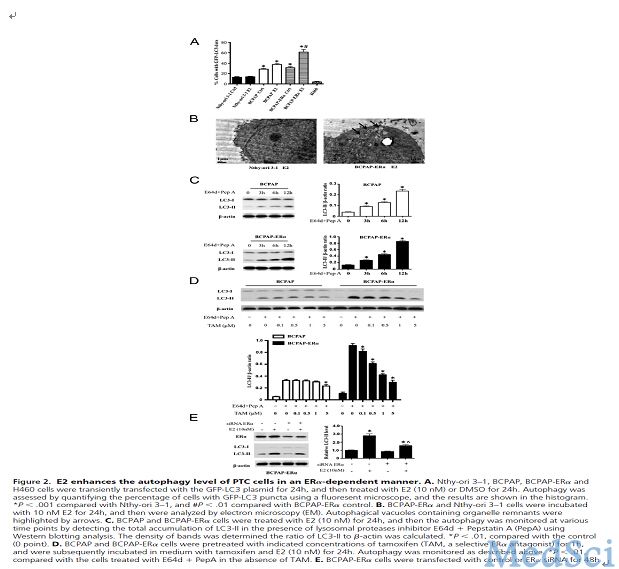
最后,研究者认为ER-α可以通过提高PTC细胞自噬水平,促进PTC细胞生长。抑制PTC细胞自噬,可能成为一种治疗ER-α阳性的PTC新方法。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCE#
53
#乳头状#
60
#JCEM#
65
#癌细胞#
67
#甲状腺乳头状癌#
71