J Periodontal Res:牙龈炎可能参与了系统性疾病的发病机制
2015-06-07 MedSci MedSci原创
菌血症,系统性炎症标记物与牙周及系统性疾病之间存在着某些联系,且有可能参与了这些疾病的发病机制。本研究旨在探究牙龈炎的发展过程中系统性炎性标记物以及菌血症的变化。研究纳入80名研究对象,根据性别、是否吸烟以及牙龈出血位点数,将其随机分成两组:对照组(n=40)和实验性牙龈炎组(n=40)。对照组每天刷牙两次,使用常规氟化钠护齿牙膏和普通手动牙刷,配合使用牙线两次/每天,漱口水(含氟化物抗龋成分)漱
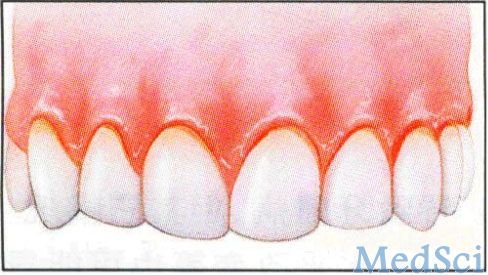
菌血症,系统性炎症标记物与牙周及系统性疾病之间存在着某些联系,且有可能参与了这些疾病的发病机制。本研究旨在探究牙龈炎的发展过程中系统性炎性标记物以及菌血症的变化。
研究纳入80名研究对象,根据性别、是否吸烟以及牙龈出血位点数,将其随机分成两组:对照组(n=40)和实验性牙龈炎组(n=40)。对照组每天刷牙两次,使用常规氟化钠护齿牙膏和普通手动牙刷,配合使用牙线两次/每天,漱口水(含氟化物抗龋成分)漱口一次。实验组停止刷牙和牙线的使用,每天仅用漱口水漱口一次,持续21天。
由于对照组中一名研究对象在试验期间使用了抗生素而被排除。整理并分析实验证据,可发现,实验组研究对象的牙菌斑水平以及牙龈炎症指数相对于基线水平明显增高。而对照组研究对象菌血症程度及可溶性细胞间粘附分子-1的水平却低于基线水平。实验性牙龈炎组,菌血症的严重程度与牙龈炎程度以及可溶性细胞间粘附分子-1的水平呈现负相关。
总而言之,实验性牙龈炎建模过程中,研究对象的系统性炎性因子的水平存在明显的差异。因此,若想探究口腔疾病是否可影响系统性疾病来解释系统性疾病的发病机制,则必须通过长期的牙周炎实验来观察研究。
原始出处:
Kinane DF, Zhang P, Benakanakere M, Singleton J, Biesbrock A, Nonnenmacher C, He T.Experimental gingivitis, bacteremia and systemic biomarkers: a randomized clinical trial.J Periodontal Res. 2015 May 9. doi: 10.1111/jre.12280.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好文章,还会关注
100
好文章,还会关注
107
#PE#
72
#系统性#
76
看看
153
看看
192
#牙龈炎#
86