改写教科书:大脑内存在淋巴管
2015-06-03 孙学军 科学网
本人1987-1992年在泰山医学院临床医学专业学习期间,我非常尊重的夏作理教授多次给我们介绍他提出的关于脑水肿淋巴管阻塞学说,他认为大脑和其他外周组织一样也存在淋巴管循环,如果淋巴管被某些病理因素阻断,可以产生淋巴回流障碍,发生特殊的脑水肿。他提出这个观点的前提就是认为大脑也存在淋巴循环,当时泰山医学院的一些教授也开展相关研究,如采用比较粗浅研究方法,证明大脑存在除血脑屏障以外的屏障比较薄弱的淋
本人1987-1992年在泰山医学院临床医学专业学习期间,我非常尊重的夏作理教授多次给我们介绍他提出的关于脑水肿淋巴管阻塞学说,他认为大脑和其他外周组织一样也存在淋巴管循环,如果淋巴管被某些病理因素阻断,可以产生淋巴回流障碍,发生特殊的脑水肿。他提出这个观点的前提就是认为大脑也存在淋巴循环,当时泰山医学院的一些教授也开展相关研究,如采用比较粗浅研究方法,证明大脑存在除血脑屏障以外的屏障比较薄弱的淋巴管系统,发现少量大分子物质能跨过血脑屏障。这不同于大脑内存在某些缺乏血脑屏障的特殊结构,可惜这些研究并没有受到广泛的关注。原因一是国内神经解剖学领域比较僵化的观念,另外一个就是缺乏比较先进的有说服力的形态学证据。这当然是比较遗憾的,不过这种大脑内存在淋巴管的思想是中国学者30年前的看法,到今天才被西方学者证明,说明我们的学者也能提出创新思路,但比较重要的是要有拿出可靠证据的技术和信心。见相关报道:Nature: 重大发现-大脑与免疫系统直接相连
2015年6月1日,《自然》杂志发表了一项惊人的,颠覆了数十年教科书的研究结果。大脑内存在淋巴管。这一发现很好的解释了T细胞和DC疫苗对脑胶质瘤有效的原因。

夏作理教授
《Nature》;Missing link found betweenbrain, immune system; major disease implications
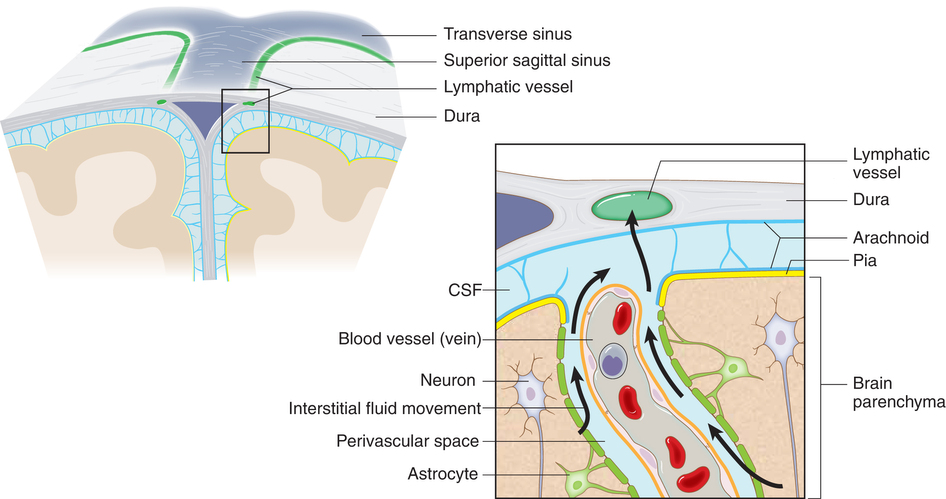
弗吉尼亚大学医学院研究人员确定了大脑是通过从前认为不存在的一些脉管直接与免疫系统相连。在全身淋巴管已彻底定位的情况下,这些脉管能逃避人们检测,这本身就令人惊讶,这一研究发现的意义则在于,将有可能对从自闭症、老年痴呆和多发性硬化等神经系统疾病的研究和治疗产生重要影响。
弗吉尼亚大学医学院神经科学教授、脑免疫学和神经胶质中心主任Jonathan Kipnis博士说:“这一研究彻底回答了大脑免疫反应是否存在,多发性硬化症患者如何会受到免疫攻击,等大脑免疫反应的基础问题。像所有其他的组织一样,大脑也可以通过脑膜淋巴管与外周免疫系统产生相互作用,这颠覆了过去关于大脑是免疫豁免器官的概念。我们相信,每个神经系统疾病都具有免疫因素,这些淋巴管或许扮演了重要角色。”
弗吉尼亚大学医学院神经科学系主任Kevin Lee说:“当我知道这些研究结果时,我只说了一句话。‘这将会改写教科书。’过去从未发现针对中枢神经系统的淋巴管。最初这一独特观察非常明确。此后他们完成了更多研究支持这一发现,这将从根本上改变人们对中枢神经系统和免疫系统关系的看法。”
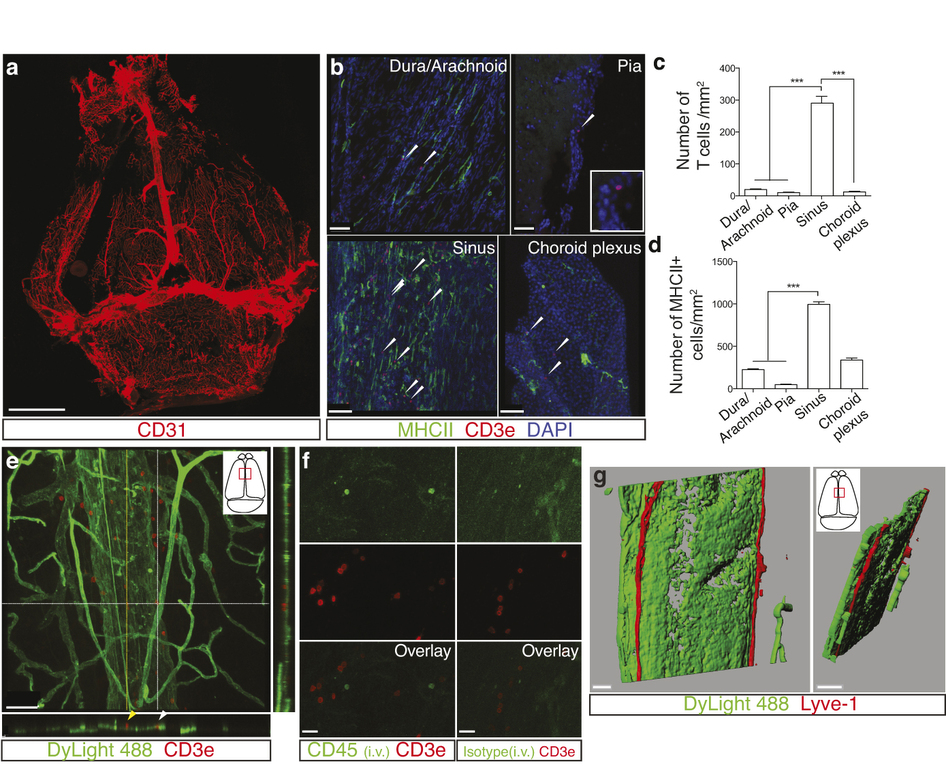
Kipnis开始持对次表示怀疑。因为他觉得似乎不可能存在目前仍然不被科学家了解的组织学结果。上世纪中叶关于组织结构的基本组成就已经完成。Kipnis实验室博士后Antoine Louveau的研究内容是这一发现的关键。Louveau开发出一种方法,可将小鼠脑膜附着到一张载玻片上,在整体检测时发现了这些淋巴管。事实上,这相当容易。只有一个窍门:只要将脑膜固定在头盖骨内,保持组织在生理状态下被固定,然后仔细分析。以其他方式不会奏效。研究发现,在载玻片上一些免疫细胞分布呈现脉管样排列,检测淋巴管特异性标记,发现确实属于淋巴管。
大脑淋巴管一直以来为什么没有被科学家注意?Kipnis认为,大脑内的淋巴管“隐藏得非常好”,它们与血管伴随进入静脉窦。这在形态学观察时难以区分。Kipnis 指出,对这些淋巴管进行活体成像是研究其功能非常重要的技术,这方面主要是神经科学助理教授Tajie Harris提供的协助。
这一意外发现对解释老年性痴呆、自闭症和多发性硬化形成的原因提供了重要信息。Kipnis 说:“如老年性痴呆,脑内累积一些蛋白质团块。有可能是因为淋巴管无法有效清除,才导致这些蛋白在大脑中累积。”他指出,这些淋巴管看起来随年龄改变,因此可能与大脑衰老过程有关。
原始出处:
Antoine Louveau, Igor Smirnov, Timothy J. Keyes, Jacob D. Eccles, Sherin J. Rouhani, J. David Peske, Noel C. Derecki, David Castle, James W. Mandell,Kevin S. Lee, Tajie H. Harris & Jonathan Kipnis.Structural and functional features of central nervous system lymphatic vessels.Nature, June 1, 2015.doi:10.1038/nature14432
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














学习了,谢谢作者分享!
123
看来又可以解决好多问题
99
厉害
99
#淋巴管#
80
长知识了!
147
zh
143