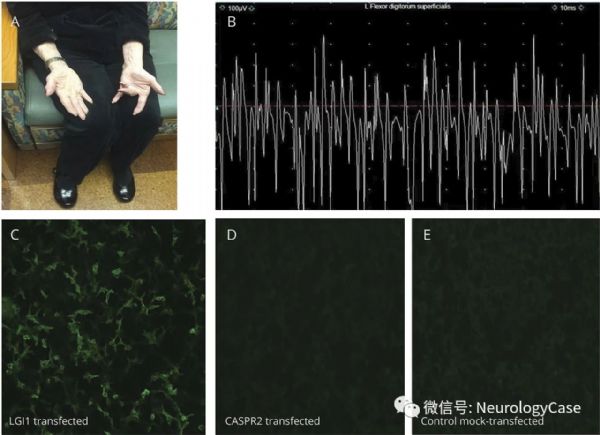
Neurology:见于LGI-1自身免疫性疾病的获得性局灶性神经性肌强直
2018-06-08 zyx整理 神经科病例撷英拾粹
81岁女性,起初被诊断为皮质基底节变性(认知功能下降和左手特殊姿势)。随后出现低钠血症和双侧面臂肌张力障碍样发作(faciobrachial dystonic seizures,FBDS)。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#神经性#
48
#Neurol#
56
#获得性#
68
#局灶性#
63
#免疫性疾病#
54
学习了.谢谢分享
83
不错的文章值得拥有.
93
谢谢分享学习
87