默克(Merck KGaA)的胆道癌疗法Bintrafusp Alfa,研究结果令人失望
2021-03-16 Allan MedSci原创
默克公司(Merck KGaA)周二宣布,Bintrafusp alfa二线治疗局部晚期或转移性胆道癌患者的试验未能达到其主要终点。
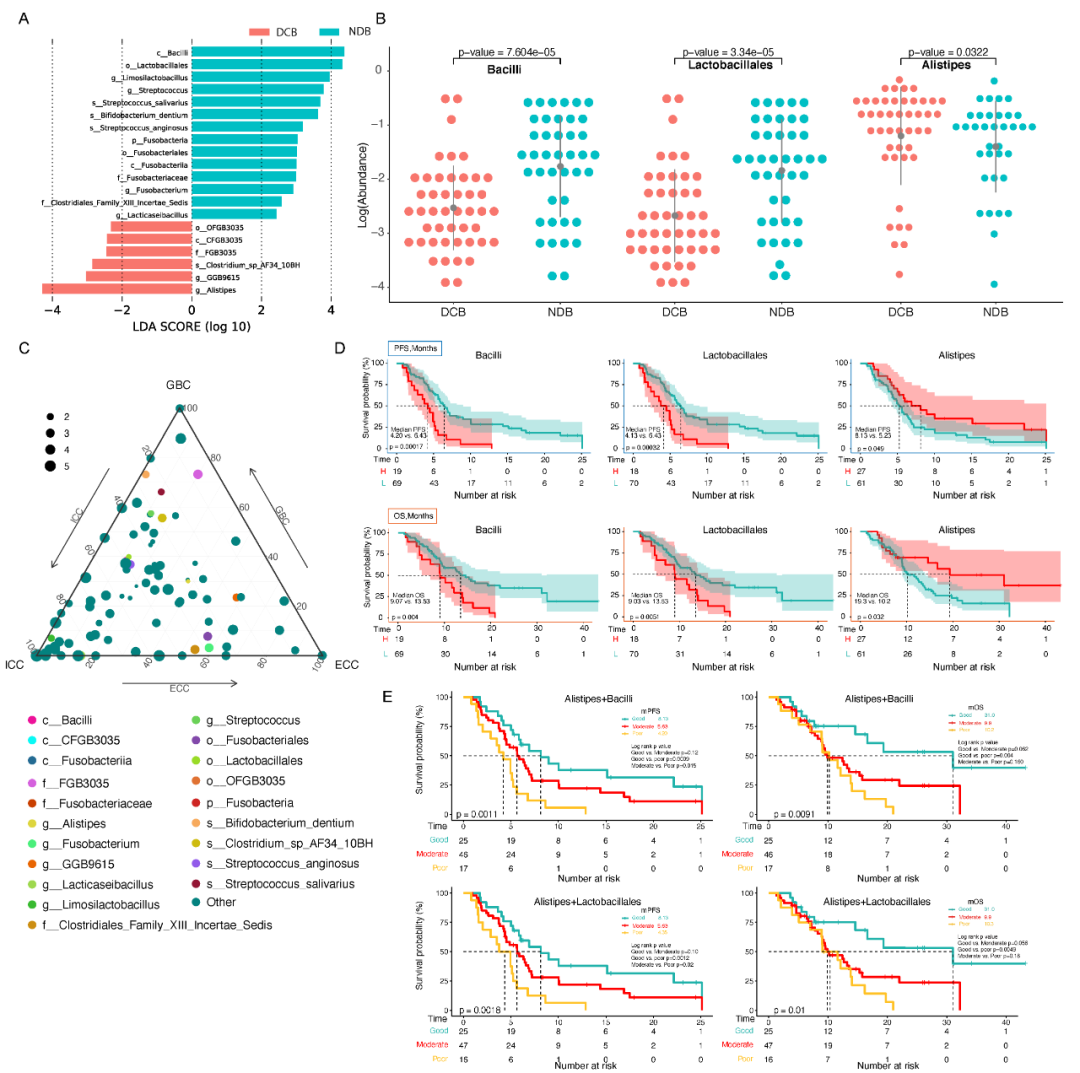
默克公司(Merck KGaA)周二宣布,Bintrafusp alfa二线治疗局部晚期或转移性胆道癌患者的试验未能达到其主要终点。该公司指出,虽然观察到双功能融合蛋白Bintrafusp alfa具有单药活性,但该研究未达到预先设定的阈值。
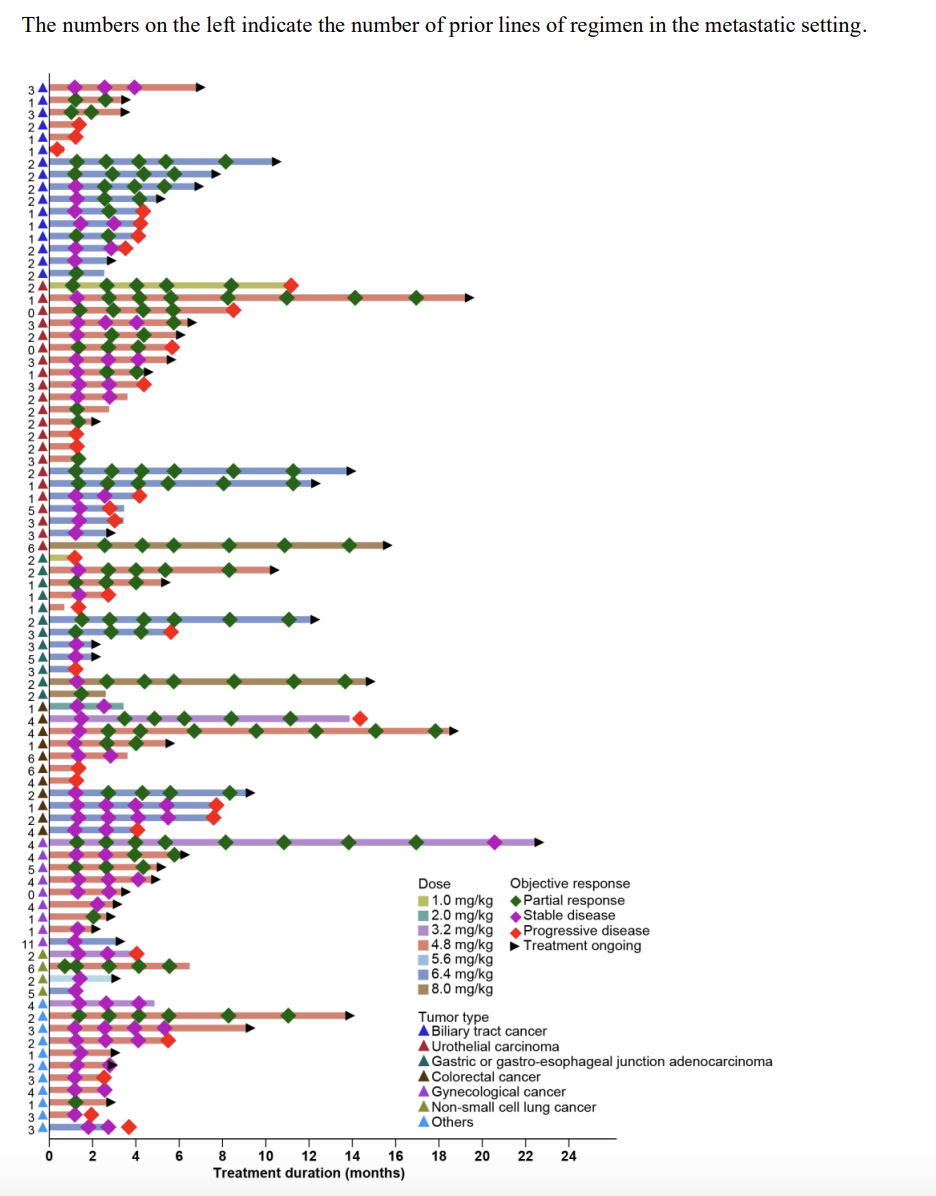
INTR @ PID BTC 047试验纳入了159例局部晚期或转移性胆道癌患者,这些患者因一线铂类化学疗法失败或无法耐受。默克公司表示,最重要的结果表明,经过九个多月的随访,bintrafusp alfa表现出了单药功效和持久性,客观缓解率(ORR)为10.1%。默克公司表示,这项研究结果将提交给即将举行的医学会议或出版物。
II / III期INTR @ PID BTC 055研究的中期阶段正在进行中,该试验正在研究将Bintrafusp alfa联合化学疗法一线治疗胆道癌的有效性和安全性。
双功能融合蛋白Bintrafusp alfa旨在阻断TGF-β和PD-L1,目前正在与葛兰素史克公司合作开发,该交易潜在价值高达37亿欧元,其中包括3亿欧元的预付款。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#ALF#
79
#Merck#
68
#研究结果#
75
#TRA#
62
#默克#
83
好文章!
126