NEJM:经皮置猪尾巴导管治疗肺栓塞-案例报道
2016-01-07 chenshuo译 MedSci原创
http://www.nejm.org/doi/full/10.1056/NEJMicm1415847
女性,77岁,因出现突发胸痛、心悸、呼吸困难4小时余被送往急诊就诊。来院时,血压测量值为60 / 40mmHg。
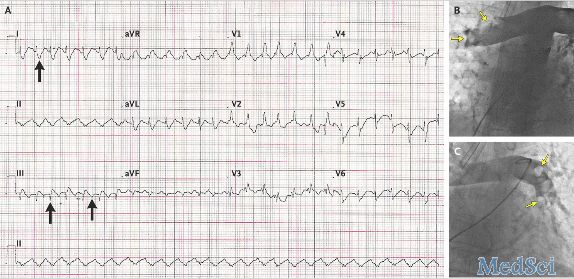
经胸行床边超声心动图检查,结果显示右心室室腔扩张,重度三尖瓣反流。
随后,该患者被送到导管实验室进行再次评估,评估结果显示她的冠状动脉未见异常。但她的双侧近端肺动脉可见广泛性血栓,最后其被诊断为肺栓塞(如图B和C,箭头所指处)。
一条型号为6-french的猪尾巴导管被送入到栓塞部位(请点击原始链接观看视频)。随后,通过猪尾巴导管对栓塞部位注入组织型纤溶酶原激活物以溶解栓塞凝块。
术后,该患者被送往ICU继续观察治疗,并应用肾上腺素药物稳定血压。此外,在术后的90分钟内再次应用组织型纤溶酶原激活剂和普通肝素进行抗凝治疗。再次经胸行床边超声心动图检查结果显示右心室功能受损,三尖瓣严重关闭不全。
Abdurrahman Oguzhan,Percutaneous Rotational Pulmonary Thrombectomy.N Engl J Med .2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













感谢分享。
141
不错,赞一个
140
这篇文章有一定深度
156
是一篇不错的文章
139
新颖
141
视觉大开
134
感谢分享
68
感谢分享
55
感谢分享
107
感谢分享
108