PLoS One:涉及岛叶皮质的缺血性卒中,可能是心源性栓塞的危险因素
2016-01-26 phylis 译 MedSci原创
目的:评估心源性脑栓塞是否与岛叶部位缺血性脑卒中相关。方法:识别症状开始7天内的住院的缺血性卒中患者。基于弥散加权成像,研究包括大脑中动脉(MCA)中缺血性病变。根据梗死是否涉及岛叶,将患者分为两组中一组。主要预后为根据是否涉及岛叶,比较心源性脑栓塞的频率。共有MCAO供血区发生缺血性卒中的患者,112名(8.5%)涉及到岛叶。与未涉及岛叶(30.4%)的患者相比,涉及岛叶卒中(52.7%)的患者
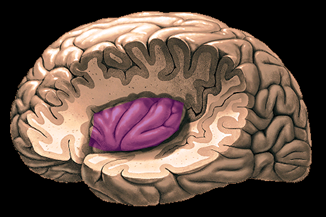
目的:评估心源性脑栓塞是否与岛叶部位缺血性脑卒中相关。
方法:识别症状开始7天内的住院的缺血性卒中患者。基于弥散加权成像,研究包括大脑中动脉(MCA)中缺血性病变。根据梗死是否涉及岛叶,将患者分为两组。主要预后为根据是否涉及岛叶,比较心源性脑栓塞的频率。
共有1311名大脑中动脉供血区发生缺血性卒中的患者,112名(8.5%)涉及到岛叶。与未涉及岛叶(30.4%)的患者相比,涉及岛叶卒中(52.7%)的患者,心源性栓塞较多。尽管,涉及岛叶与基线严重的NHISS分数相关(13 vs 4),但它并不能影响3个月功能预后。
结论:在MCA供血区缺血的卒中患者,涉及岛叶皮质可能是心源性栓塞的危险因素。
Kang J, Hong JH, et al.Cardioembolism and Involvement of the Insular Cortex in Patients with Ischemic Stroke.PLoS One. 2015 Oct 21.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Plos one#
83
#缺血性卒#
76
#缺血性#
69
#心源性#
71
这篇文章有深度
127
这篇文章有一定深度
103
是一篇不错的文章
143
看不懂
104