J Microbiol:粪肠球菌CBT SL-5精华液或可能为治疗轻中度痤疮的新选择
2022-05-18 sunshine MedSci原创
寻常性痤疮是一种多因素的疾病,其特点是皮脂分泌过多、毛囊角质化、痤疮杆菌在毛囊角质层的定植以及炎症。抗生素耐药的痤疮杆菌和皮肤微生物组的失调在痤疮治疗中越来越受到关注。
寻常痤疮是一种多因素的疾病,其特点是皮脂分泌过多、毛囊角质化、痤疮杆菌在毛囊角质层的定植以及炎症。抗生素耐药的痤疮杆菌和皮肤微生物组的失调在痤疮治疗中越来越受到关注。粪肠球菌是一种广泛使用的益生菌,通过对痤疮丙酸杆菌发挥抗菌活性而显示出对痤疮治疗的好处。近日,发表于J Microbiol的一项随机对照试验探究了粪肠球菌CBT SL-5精华液对轻度至中度痤疮患者的疗效和安全性。
研究共纳入了20名患者参加了这项随机、安慰剂对照、分脸对比研究。患者在一侧脸部使用粪肠杆菌洗剂,另一侧使用载体洗剂,治疗4周。疗效评估措施包括调查人员对痤疮严重程度的评估、患者满意度、皮肤参数的变化和皮肤微生物组的多样性的改善。
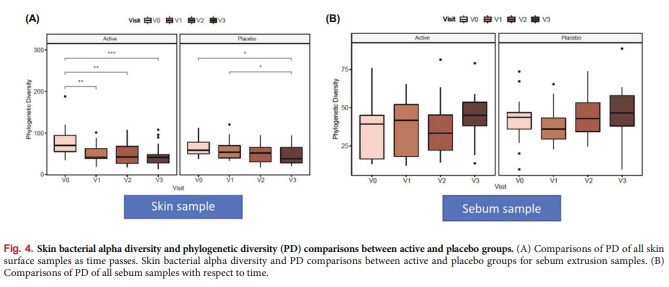
结果显示,干预处理2周(p = 0.009)和6周(p < 0.0005)后,与对照组相比,测试组患者的调查人员评估得分有明显改善。然而,两组之间的TEWL和皮肤水合度没有明显差异。测试组患者的皮肤样本中,皮肤微生物群的系统发育多样性随时间推移而减少。
综上所述,该研究结果表明,粪肠球菌CBT SL-5提取物可以成为改善轻度至中度痤疮患者的痤疮严重程度和皮肤微生物群失调的一个可行且耐受性良好的选择。基于这些结果,在建议更广泛地使用之前,需要进一步设计更多的样本量和更长的随访期的大型研究来加以验证。
原始出处:
Hye Sung Han, et al., A split face study on the effect of an anti-acne product containing fermentation products of Enterococcus faecalis CBT SL-5 on skin microbiome modification and acne improvement. J Microbiol. 2022 May;60(5):488-495. doi: 10.1007/s12275-022-1520-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Biol#
86
#Bio#
76
#CRO#
80
#Micro#
69
#肠球菌#
69
#粪肠球菌#
73
#CBT#
79