JSDT:椎间盘突出融合术的长期疗效于椎间盘切除术相似
2014-06-30 orthop217 丁香园
不融合的单纯部分椎间盘切除术(间盘切除)为治疗椎间盘突出下肢放射痛的标准方法。但由于椎间盘为脊柱运动单元的生物力学稳定装置,学者认为椎间盘切除术后节段不稳为残余腰痛和椎间盘突出复发的危险因素。目前有多种融合技术,包括PLIF,TLIF,这些新技术融合了原发性椎间盘突出节段。 而单侧椎间盘切除术与融合术两者长期随访疗效的研究,相对较少。 日本福岛医科大学医学院骨科的学者进行了一项回顾
不融合的单纯部分椎间盘切除术(间盘切除)为治疗椎间盘突出下肢放射痛的标准方法。但由于椎间盘为脊柱运动单元的生物力学稳定装置,学者认为椎间盘切除术后节段不稳为残余腰痛和椎间盘突出复发的危险因素。目前有多种融合技术,包括PLIF,TLIF,这些新技术融合了原发性椎间盘突出节段。
而单侧椎间盘切除术与融合术两者长期随访疗效的研究,相对较少。
日本福岛医科大学医学院骨科的学者进行了一项回顾性长期随访研究,明确了椎间盘突出融合术的长期疗效等同于单侧椎间盘切除术,文章于2014年6月发表在J Spinal Disord Tech上。
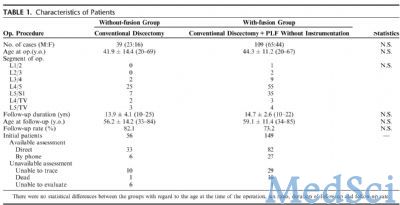
该回顾性研究病例包括两组,单侧椎间盘切除的39病例来自A医院,平均年龄41.9岁,平均随访时间13.9年;椎间盘切除+非内固定的后外侧融合术(当时无内固定)的109例来自B医院,平均年龄44.3岁,平均随访时间15年。两组病例在年龄,性别分布,随访时间和随访率上无统计差异(表1)。
表1 两组病例的特点对比
评估的指标包括主观症状:镇痛药使用,持续行走时间,改良的四分级疗效标准(优,良,中,差),疼痛数字量表,手术满意度,Roland-Morris残障指数问卷日语版。客观症状包括:直腿抬高试验,手动肌力测试,感觉障碍。
结果显示,两组间在主观和客观指标方面均无明显统计学差异(表2,表3,表4)。两组病例翻修手术例数亦无明显统计学差异(表5)。
表2 单侧间盘切除和切除+融合病例主观指标对比。
两组间无明显统计差异,而融合组13%的病例有取骨相关症状
表3 单侧间盘切除和切除+融合病例基于患者的评估对比
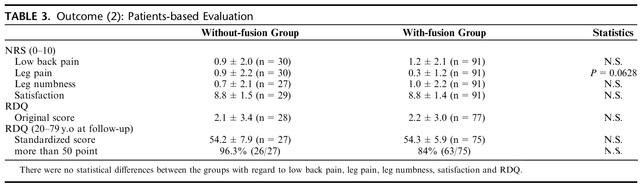
表4 单侧间盘切除和切除+融合病例阳性体征对比
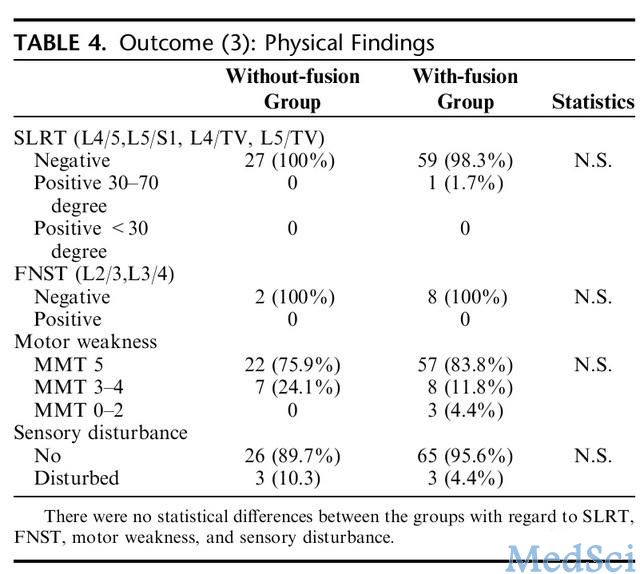
表5 单侧间盘切除和切除+融合病例翻修手术对比

以上结果表明,就长期疗效而言,椎间盘切除+融合术并不比单纯椎间盘切除术优越。单纯椎间盘切除术与椎间盘切除+融合术长期疗效相当。
目前椎间盘切除术为保守治疗失败的椎间盘突出手术治疗的金标准,包括传统的开窗减压,髓核摘除术;微创椎间盘镜下椎间盘切除术。传统的椎间盘切除长期疗效确实,但椎间盘镜下间盘切除术长期疗效未知。
自1996年美国FDA批准使用椎间融合器后,融合技术迅猛发展。但融合能否改变椎间盘突出的长远疗效?尽管本研究所用的融合技术过时,但确实给我们提供了很好的信息。平均14年的随访,有力的说明了融合并不能改善椎间盘突出患者的长期疗效。
尽管融合可防止该节段的椎间盘突出复发,但由融合带来的邻近节段退变而翻修的病例,并不必单纯做复发的病例少。
原始出处:
Otani K1, Kikuchi S, Sato K, Yabuki S, Yamauchi K, Takeyachi Y, Konno S.Does the Fusion of a Lumbar Disk Herniation Improve the Clinical Outcome? An Investigation With a Minimum 10-Year Follow-up.J Spinal Disord Tech. 2014 Jun;27(4):196-201. doi: 10.1097/BSD.0b013e318269399c.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#切除术#
57
#椎间盘突出#
56
#融合#
68
#融合术#
60
#长期疗效#
63