脊髓灰质炎疫苗常见问题解答
2016-05-03 卫计委 卫计委
第一部分 疾病简介 1. 什么是脊髓灰质炎? 脊髓灰质炎(简称脊灰)是由脊灰病毒引起的传染病,多发生于儿童,故俗称为“小儿麻痹症”。感染者可能出现肢体麻痹,出现麻痹的病例多数留下跛行等终生致残。 脊灰病毒按其抗原性不同,分为Ⅰ型、Ⅱ型、Ⅲ型共3个血清型。 2. 脊灰病毒的传染源和传播途径是什么?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





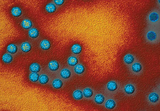




#脊髓灰质炎疫苗#
74
文章真心很好,感谢作者
98
深入学习,好文值得点赞!
108
中国真的需要普及一下基本的资料知识
178
很不错,但是希望广大群众也看下
118
学习啦,不错
22
仔细阅读
164
#常见问题#
55
#脊髓灰质炎#
92
这篇文章写的很详细,非常好
105