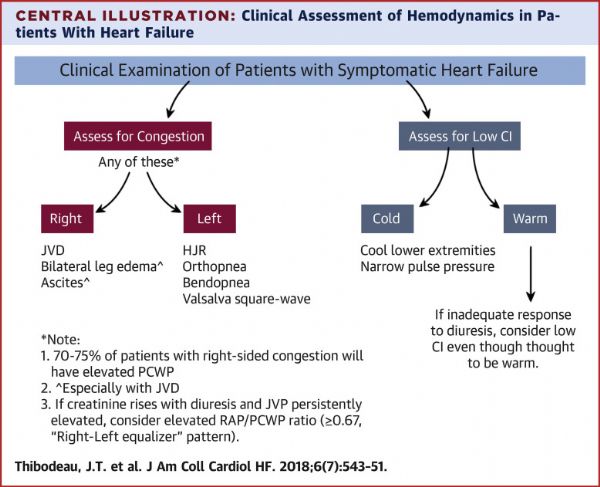
JACC Heart Fail:一图读懂心衰体检,九个体征可了解体循环淤血、肺淤血和低心排情况
2018-07-04 文韬 中国循环杂志
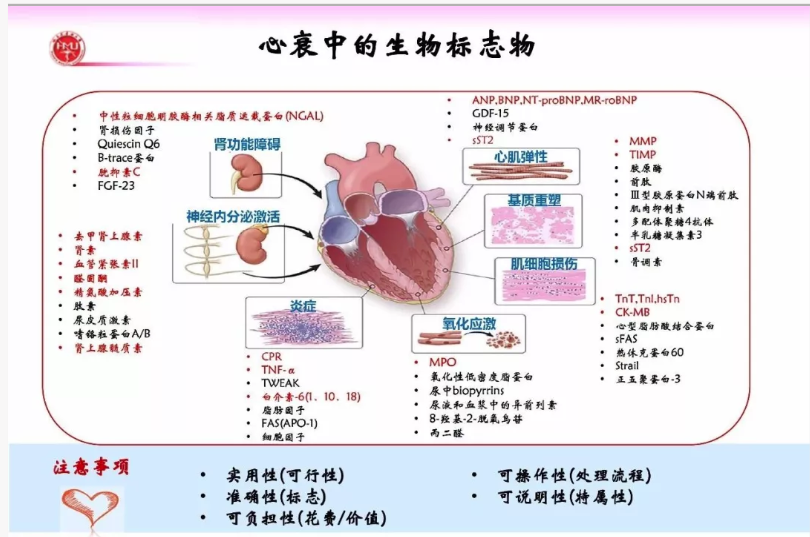
JACC心衰子刊评述了目前心力衰竭体格检查。文章指出,尽管生物标志物和技术取得了进步,但病史和体格检查仍然是心力衰竭患者管理的基石。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
63
心衰患者评估.
109
学习并分享!!
103
学习了谢谢分享!!
81
学习了.获益匪浅.感谢分享
104
#体检#
52
#ACC#
55
#ART#
58
#HEART#
58
心脏衰竭的治疗.
0