European Radiology:如何通过影像学对甲状腺乳头状癌患者进行风险分层?
2022-06-21 shaosai MedSci原创
研究表明,约30-80%的PTC患者可能有中心淋巴结转移(CLNM)。CLNM阳性的患者可能有较高的一侧LNM(LLNM)风险是与复发相关的危险因素,也是影响手术方法和预后评价的决定因素。
由于早期诊断和成像技术的进步,甲状腺癌的发病率持续上升。分化型甲状腺癌占95%以上,主要病理类型为甲状腺乳头状癌(PTC),其总体预后最好。研究表明,约30-80%的PTC患者可能有中心淋巴结转移(CLNM)。CLNM阳性的患者可能有较高的一侧LNM(LLNM)风险是与复发相关的危险因素,也是影响手术方法和预后评价的决定因素。
在甲状腺癌的治疗中,预防性的LNN清扫(CLND)是否有必要是一个关键且有争议的问题。考虑到LNs阳性的高风险,一些研究者建议将PTC的常规CLND作为初始手术以获得更好的治疗效果。然而,2015年美国甲状腺协会指南并不推荐预防性的CLND,表明CLNM和LLNM一般需要治疗性的CLND。因此,术前准确、全面地评估LNM的风险以促进手术决策是非常重要的。
鉴于超声(US)的高分辨率、便捷性和无创性,可以作为术前评估原发性甲状腺肿瘤和颈部LN的主要影像学手段。然而,由于受到颈部中央解剖结构的影响,US在检测CLNM方面的能力有限。
近日,发表在European Radiology杂志的一项研究探讨了与PTC相关的LNM的预测因素,并结合术前多模态US和临床特征建立了易于临床操作的列线图以用于直观和定量的对CLNM进行预测。
共有822名PTC患者被纳入本项回顾性研究。本研究构建了甲状腺肿瘤超声模型(TTUM)和甲状腺肿瘤和LLN超声模型(TTCLNUM)作为列线图来预测CLNM风险。使用AUCs评估了模型的性能。校准和决策曲线被用于评估准确性和临床效用。
对于TTUM训练和测试集,AUCs分别为0.786和0.789,偏差校正后的AUCs为0.786和0.831。对于TTCLNUM训练和测试集,AUCs分别为0.806和0.804,偏差校正后的AUCs为0.807和0.827。TTCLNUM列线图的校准和决策曲线显示了更高的准确性和临床实用性。当US肿瘤大小≤8.45毫米时,训练集和测试集的AUC分别为0.746和0.719,特异性为0.942和0.905;而当肿瘤大小>8.45毫米时,AUC为0.737和0.824,敏感性为0.905和0.880。
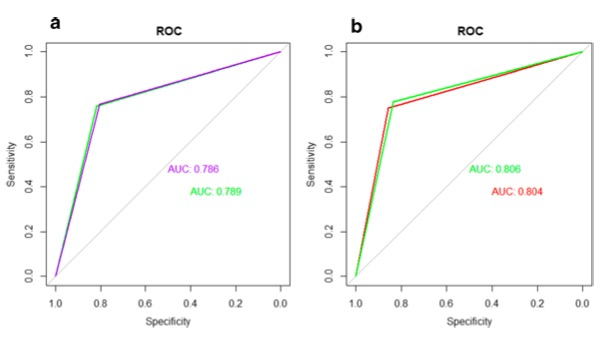
图 a TTUM在训练集(紫色曲线)和测试集(绿色曲线)中的ROC曲线。 b TTCLNUM在训练集(绿色曲线)和测试集(红色曲线)中的ROC曲线
本项回顾性研究发现,男性、年龄较小、C-TIRADS分类较高、弹性成像得分较高、囊性关系不明确、肿瘤位于深部、异质回声、同侧多发、弥漫性微钙化、Alder分级较高、发现可疑CLN、LLN与非LN或混合CDFI这些征象会增加PTC患者的CLNM风险。基于多模态US成像和临床数据的列线图可用于术前CLNM的风险评估,为主动监测和治疗决策提供有价值的信息。
原文出处:
Quan Dai,Dongmei Liu,Yi Tao,et al.Nomograms based on preoperative multimodal ultrasound of papillary thyroid carcinoma for predicting central lymph node metastasis.DOI:10.1007/s00330-022-08565-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#乳头状#
87
#PE#
69
#甲状腺乳头状癌患者#
77
学习一下
72
认真学习了
79
#风险分层#
76
#甲状腺乳头状癌#
68