AACR 2015:七大癌症研究热门新技术
2015-05-07 佚名 生物谷
在刚刚结束的费城2015年AACR(全美癌症研究者协会)会议上,著名生命科学网站SelectScience公布了“七大癌症研究热门新技术”名单,提名了细胞能量代谢检测、循环肿瘤细胞检测等新技术、新平台。1. 蔡司ZEISS配有Airyscan的 LSM880 获得 Life Science Scientists' Choice 奖项SelectScience宣布蔡司ZEISS配有Airy
在刚刚结束的费城2015年AACR(全美癌症研究者协会)会议上,著名生命科学网站SelectScience公布了“七大癌症研究热门新技术”名单,提名了细胞能量代谢检测、循环肿瘤细胞检测等新技术、新平台。
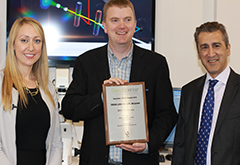
1. 蔡司ZEISS配有Airyscan的 LSM880 获得 Life Science Scientists' Choice 奖项
SelectScience宣布蔡司ZEISS配有Airyscan的LSM880因被评为2014年最佳新生命科学产品而成为2015年科学家选择奖®的获得者。
2. XF平台与试剂盒 - Seahorse Bioscience
全新的XFp小型系统和细胞能量代谢表型检测试剂盒,可以快速、一次性确定细胞当前线粒体有氧呼吸和糖酵解两条途径的能力与潜力(细胞向外界压力做出反应的能力)。通过同时测量基础和压力状态下的两大能量代谢途径的相对利用率,研究人员现在可以快速地发现基因变化对代谢的影响。例如,XFp细胞能量代谢测试可以很容易地考察代谢与肿瘤生存和Ras致癌基因之间的联系。含有Ras致癌基因的肿瘤,其能量代谢表型显示为在压力状态下对葡萄糖的明显依赖,揭示了生存在缺氧和酸性环境中肿瘤的代谢弱点。
3. 新数据识别EKF PointMan技术评估肺癌突变状态--EKF诊断
EKF诊断日前宣布,其PointMan™DNA浓缩技术已被确认为一个简单而有效的方法进行非侵入性判断晚期肺癌患者的血浆EGFR T790M突变状态。
4. 首个全一体光谱仪/荧光系统 - Denovix
DeNovix公司在今年的美国癌症治疗协会(AACR2015)会议上推出DS-11 FX+光谱仪/荧光系统。
5. 卵巢癌的早期发现:维也纳医科大学演示“血活检”技术-- ANGLE plc
维也纳医科大学的研究人员在美国癌症研究协会年度会议上发表了科学海报,详细介绍了与定量PCR相结合的新型微流体Parsortix™技术流程,实现了分子水平上循环肿瘤细胞(CTCs)对卵巢癌和乳腺癌影响的分析。
6. 针对癌症免疫学研究的Mantra™定量病理成像系统--珀金埃尔默PerkinElmer
珀金埃尔默公司在2015年美国临床研究协会年度会议上宣布其癌症研究解决方案,包括Mantra™定量病理工作站与inFORM®图像分析软件。
7. 实时荧光定量PCR系统将研究人员在云端进行连接--Thermo Fisher Scientific
新的实时PCR系统,随着与云计算技术全面整合,如Applied Biosystems公司QuantStudio 3和QuantStudio 5实时PCR系统,标志着数据共享和全球研究合作的新时代。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很高
138
很有用
186
#新技术#
54
#ACR#
74
#癌症研究#
59
#AACR#
62