Oral Oncol:HPV感染可促使年轻个体头颈癌的发生率升高
2015-06-21 MedSci MedSci原创
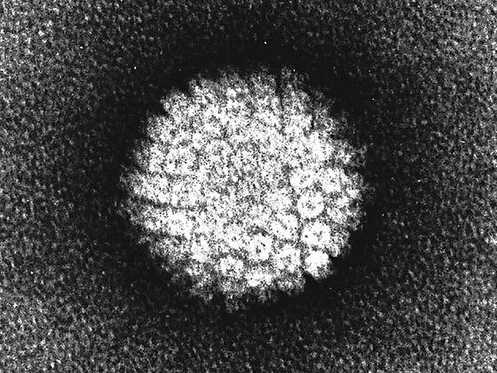
Oral Oncol:HPV感染可促使年轻个体头颈癌的发生率升高 在过去的30年里,头部和颈部肿瘤的面貌发生了巨大的变化。与烟草和酒精相关的鳞状细胞癌在过去的30年里稳步下降,但是与人乳头瘤病毒(HPV)相关的肿瘤发病率却逐渐增加,且较易发生在40-50岁的非吸烟人群中。有研究表明,约70-90%的新发口咽癌存在HPV感染。有研究表明,一生中口交伴侣(>5)以及阴道性交伴侣(>25)较高与HPV阳

在过去的30年里,头部和颈部肿瘤的面貌发生了巨大的变化。与烟草和酒精相关的鳞状细胞癌在过去的30年里稳步下降,但是与人乳头瘤病毒(HPV)相关的肿瘤发病率却逐渐增加,且较易发生在40-50岁的非吸烟人群中。有研究表明,约70-90%的新发口咽癌存在HPV感染。
有研究表明,一生中口交伴侣(>5)以及阴道性交伴侣(>25)较高与HPV阳性头颈癌患者的高风险有关。人们可以在性活跃年龄之前通过接受HPV疫苗免疫以降低HPV相关的头颈癌发生的风险。
最近的证据表明,相对于烟草相关性头颈癌,HPV相关的头颈癌可表现出多种不同的症状。HPV最流行的检测方法为p16免疫组化染色,廉价且简单,研究表明它较以往的标准检测方法灵敏性和特异性高。现在普遍建议所有口咽癌患者进行HPV检测,有些地方甚至建议所有头颈癌患者均应进行HPV检测。
HPV阳性的头颈癌患者的2年和5年总生存率明显高于HPV阴性的头颈癌患者,这可能是由于HPV阳性的肿瘤对治疗反应更为灵敏。
原始出处:
Young D, Xiao CC, Murphy B, Moore M, Fakhry C, Day TA.Increase in head and neck cancer in younger patients due to human papillomavirus (HPV).Oral Oncol. 2015 Jun 8. pii: S1368-8375(15)00182-7. doi: 10.1016/j.oraloncology.2015.03.015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好文章,还会关注
117
这个,还是值得深入研究的
157
在国内少有医院对口腔癌患者常规查HPV
172
#Oral#
63
#发生率#
57
#Oncol#
62
#头颈癌#
63
#HPV感染#
76
中国相对减少
170
这个主要是老外
161