EHJ-Acute CardioVascular Care:再论STEMI患者的“血脂悖论”,基于中国心血管疾病医疗质量改善项目的发现
2021-12-14 “心关注”公众号 “心关注”公众号
近年来由于社会老龄化加剧,心血管病危险因素增多,急性心肌梗死(MI)发病率及死亡率不断攀升,造成了巨大的经济负担,因此控制冠状动脉性心脏病(CAD)患者死亡危险因素成为当下治疗热点。
近年来由于社会老龄化加剧,心血管病危险因素增多,急性心肌梗死(MI)发病率及死亡率不断攀升,造成了巨大的经济负担,因此控制冠状动脉性心脏病(CAD)患者死亡危险因素成为当下治疗热点。低密度脂蛋白胆固醇(LDL-C)是动脉粥样硬化的始动因素,是斑块形成及破裂的核心机制,一系列研究表示CAD患者接受降脂治疗后可显着降低心血管事件风险。但近几十年既往研究发现LDL-C水平与MI后的临床结局呈负相关。天津医科大学总医院心内科杨清/周欣团队一项观察性研究同样发现极低LDL-C水平与急性冠脉综合征患者强化抗栓治疗期间院内出血风险的增加有关。另外,基础研究显示,胆固醇与磷脂结合构成细胞外膜的基本骨架,调节细胞膜的流动性并维护细胞膜稳定,在人体中的作用不容忽视。
目前对急性心肌梗死患者的低脂相关死亡风险仍未有定论,以及对不同人群用药剂量及种类是否有明显差别都是当下医疗亟待解决的问题。这可能影响医师对ACS患者的他汀应用问题。因此,在人群水平阐明入院LDL-C水平与ST段抬高型心肌梗死(STEMI)患者院内死亡率的剂量-反应关系具有重要的临床意义。
图1. 天津医科大学总医院心内科杨清/周欣团队European Heart Journal Acute CardioVascular Care论文首页
2021年12月6日,该团队的论着“Revisiting the lipid paradox in ST-elevation myocardial infarction in the Chinese population: findings from the CCC-ACS project” 在欧洲心脏杂志子刊(European Heart Journal-Acute CardioVascular Care; 2020 JCR IF 4.696)在线发表(图1)11。该研究基于中国心血管疾病医疗质量改善(CCC-ACS)项目,研究结果显示STEMI患者入院LDL-C水平与院内死亡风险无关。先前报道的MI患者入院时LDL-C水平与STEMI患者院内死亡率之间的负相关可能是混杂因素控制不足导致的。在2014年至2019年从全国240家参与医院招募的44563例STEMI患者中,该研究分析了入院LDL-C水平与院内全因死亡的剂量-反应关系,在对入院前变量、PCI相关变量和双联抗血小板治疗状态、入院24小时内的其他院内药物(如以他汀类药物、β受体阻滞剂和ACEI/ARB为代表的指南指导的药物治疗(GDMT)的相关药物)共计43个协变量进行多变量校正后,STEMI患者入院LDL-C水平与院内死亡风险无统计学上的相关性(图2)。

图2. 在多变量校正前,当STEMI患者LDL-C水平低于75 mg/dL时,住院死亡率显着增加(A)。但在逐步校正入院前特征(B)、PCI相关临床变量(C)后,LDL-C相关阈值从75 mg/dL分别降至70 mg/dL和65 mg/dL,最终在加入其他院内用药的完全校正模型(D)中统计学意义消失(限制性立方样条)。
在图2B中,校正入院前变量(人口学特征、并发症、入院前药物和既往病史)后,LDL-C处于70 mg/dL以下范围时与院内死亡风险增加有统计学相关性。这一发现表明,在接受院内治疗方案之前,入院LDL-C < 70 mg/dL的STEMI患者院内死亡风险显着高于入院LDL-C ≥ 70mg/dL的患者。因此,该文章以LDL-C阈值70 mg/dL为分界线,比较了研究结果在不同人群的稳健性。如图3所示,排除伴有ASCVD既往病史、入院时Killip IV、院前口服他汀类药物、入院48小时内死亡或院前曾接受溶栓的患者后,LDL-C < 70 mg/dL的相关风险是一致的。值得注意的是,排除存在GDMT药物禁忌症和症状至入院时间延长(≥ 6小时)的患者后,LDL-C < 70 mg/dL与院内死亡之间的相关性减弱,结果提示及时服用指南指导的药物、提前接触医学治疗和冠脉灌注可能改变低入院LDL-C水平的院内相关风险。
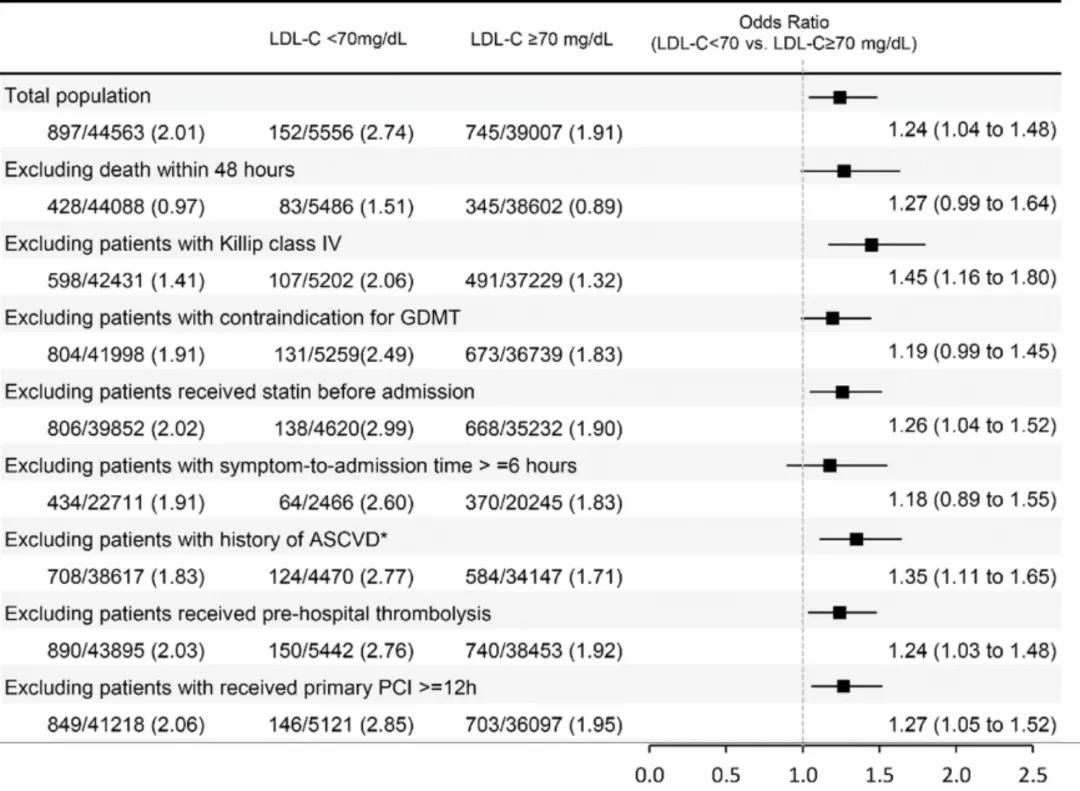
图3.LDL-C<70 mg/dL与≥70 mg/dL患者的敏感性分析
该杂志同时配发的评论12认为尽管该研究存在过度校正的风险,但根据研究结果显示,LDL-C水平较低与STEMI严重程度存在相关性的假说可能并不具备生物学基础。入院时LDL-C水平与住院死亡率之间的联系由于其他潜在的混杂因素可能存在因果倒置,解决这项问题的关键在于确定LDL-C水平与入院患者病情严重程度的关系。虽然仍需进一步深入研究分析这些机制才能彻底揭开“血脂悖论”的神秘面纱,但毫无疑问这项研究已经掀开了其中一角。
综上,该研究结果显示并不支持目前STEMI患者中存在院内全因死亡率方面的“脂质悖论”,即STEMI患者入院LDL-C水平与院内死亡风险无关。同时,该研究也提示在接受GDMT治疗的STEMI患者中,LDL-C水平不应作为患者病情恶化的因素而影响降脂药物的应用。
原始出处:
Haonan Sun, Ziping Li, Xiwen Song, et al. Revisiting the lipid paradox in ST-elevation myocardial infarction in the Chinese population: findings from the CCC-ACS project. European Heart Journal. Acute Cardiovascular Care, Volume 10, Issue 9, December 2021, Pages 978–987, https://doi.org/10.1093/ehjacc/zuab053.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#质量改善#
78
#vascular#
90
#ASC#
67
#STEMI患者#
151
#医疗质量#
92
#Acute#
99
#STEM#
91
#血管疾病#
73
#cardiovascular#
0