Nature Medicine:免疫疗法在多发性骨髓瘤治疗中取得重大成功
2015-07-21 何嫱 译 生物通
近年来,免疫疗法成为了一种有前景的癌症治疗方法。遗传改造患者自身的免疫细胞来靶向肿瘤,现在这一策略在对当前无法治愈的一种恶性浆细胞疾病——多发性骨髓瘤的治疗中取得了重大成功。相关的研究结果发布在《自然医学》(Nature Medicine)杂志上。 患者在接受了自体干细胞移植后,体内再度被输入大约24亿个遗传改造T细胞。20名晚期患者其中的16人产生了显著的临床反应。科学家们发现患者能 够普遍
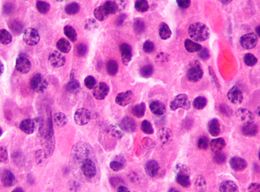
近年来,免疫疗法成为了一种有前景的癌症治疗方法。遗传改造患者自身的免疫细胞来靶向肿瘤,现在这一策略在对当前无法治愈的一种恶性浆细胞疾病——多发性骨髓瘤的治疗中取得了重大成功。相关的研究结果发布在《自然医学》(Nature Medicine)杂志上。
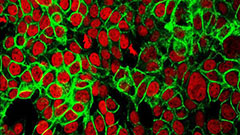
患者在接受了自体干细胞移植后,体内再度被输入大约24亿个遗传改造T细胞。20名晚期患者其中的16人产生了显著的临床反应。科学家们发现患者能 够普遍很好地耐受这一T细胞治疗,遗传改造免疫细胞移行到了骨髓处显示出长期的抗肿瘤能力。肿瘤复发通常与工程T细胞丧失有关。
论文的第一作者、马里兰大学医学院医学肿瘤学教授Aaron P. Rapoport博士说:“这一研究表明利用遗传工程T细胞进行治疗不仅安全,并在某些类型侵袭性多发性骨髓瘤患者中显示出潜在的临床效益。我们的研究结 果为在骨髓瘤细胞免疫治疗领域开展进一步的研究,帮助我们的患者取得更好的结果奠定了坚实的基础。”
这项试验是第一次报道利用遗传工程T细胞来治疗多发性骨髓瘤患者。Rapoport说,过去曾利用了这种方法来治疗白血病和淋巴瘤。
在美国有7.7万多人罹患多发性骨髓瘤,每年新确诊病例达2.4万人。患者只能接受化疗及自体干细胞移植,但这些疗法的长期反应率低,患者平均生存时间为3-5年。
Rapoport博士写道:“大多数参与这项试验的患者都获得了有意义的临床效益。其中一些患者在近3年后仍然处于缓解期。”
在这项临床研究中,研究人员操控患者的T细胞表达了针对肿瘤抗原——癌症睾丸抗原(CT抗原)的特异性受体:亲和力增强的T细胞受体(TCR)。这 里的靶CT抗原是NY-ESO-1和LAGE-1。研究报道,高达60%的晚期骨髓瘤表达NY-ESO-1和/或LAGE-1,这与肿瘤的增殖及预后不良 之间存在关联。根据Adaptimmune公司所说,这一试验是第一次报告在人体中研究慢病毒载体介导的TCR基因表达。
在20名接受治疗的患者中,14人(70%)在治疗后三个月内接近完全缓解或是完全缓解。中值无进展存活期为19.1个月,总生存期为32.1个 月。两名患者在治疗后三个月获得了极好的部分反应。作者们提到反应率要好于标准自体干细胞移植。并且,没有任何患者出现巨细胞活化综合征或细胞因子释放综 合征——在其他癌症试验中观察到的输注反应,表现为发烧、恶寒、低血压或皮疹。未出现任何与治疗相关的死亡。
马里兰大学医务部副院长、马里兰大学医学院著名教授E. Albert Reece说:“多发性骨髓瘤是一种可治疗但却基本无法治愈的癌症。这项研究揭示了采用遗传工程T细胞进行免疫治疗有望增强机体对癌症的攻击能力,为患者提供更好的治疗及控制他们的疾病。”
原始出处:
Aaron P Rapoport et al.NY-ESO-1–specific TCR–engineered T cells mediate sustained antigen-specific antitumor effects in myeloma.Nature Medicine.July 20, 2015.doi:10.1038/nm.3910
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
50
#DIC#
55
#多发性#
63
#CIN#
62
#Medicine#
52
#Med#
41