Lancet:颈椎椎体骨赘引发小脑梗死一例
2014-05-20 伊文 丁香园
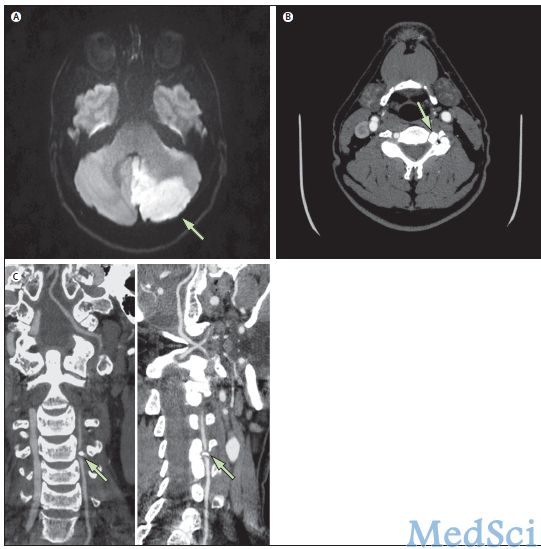
图A:弥散加权MRI示小脑后下动脉急性梗死;图B:CT血管造影示由颈椎椎体骨赘造成的外源性压迫左侧椎动脉;图C:三维CT血管造影重塑的矢状面和冠状面示左侧椎动脉外源性压迫。 该病例摘自近期The Lancet,由Ozlem Ozkul-Wermester博士等发表。 患者男,59岁,因“突发头晕、头痛、恶心及左手活动笨拙”就诊。神经系统检查示多向性眼球震颤和左侧运动
该病例摘自近期The Lancet,由Ozlem Ozkul-Wermester博士等发表。
患者男,59岁,因“突发头晕、头痛、恶心及左手活动笨拙”就诊。神经系统检查示多向性眼球震颤和左侧运动性小脑综合征。患者无颈部受伤史。头部MRI示左侧小脑后下动脉急性梗死。CT血管造影示第4颈椎上关节突的骨赘压迫左侧椎动脉,使其在颅外穿过横突孔时造成狭窄。
椎动脉外源性压迫是颈椎椎体骨赘非常罕见的并发症,栓塞性脑梗死很少发生。切除骨赘,解除椎动脉压迫是常用的外科治疗手段。
原始出处:
Ozlem Ozkul-Wermester, Dr Romain Lefaucheur,Bertrand Bourre.Cervical osteophyte causing cerebellar infarction.Lancet,17 May 2014 doi:10.1016/S0140-6736(13)61786-9
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
67
#椎体#
65
#脑梗#
105