Cell Prolif:SFRP2可增强缺氧和炎症条件下间充质干细胞的成骨/成牙分化
2020-10-07 MedSci原创 MedSci原创
基于间充质干细胞(MSC)的牙科组织再生是未来一种潜在的治疗方法,而炎症和缺氧状态会影响MSC介导的组织再生。本研究拟探讨炎症和缺氧条件下,分泌的卷曲相关蛋白2(SFRP2)对间充质干细胞功能的影响及
基于间充质干细胞(MSC)的牙科组织再生是未来一种潜在的治疗方法,而炎症和缺氧状态会影响MSC介导的组织再生。本研究拟探讨炎症和缺氧条件下,分泌的卷曲相关蛋白2(SFRP2)对间充质干细胞功能的影响及机制。
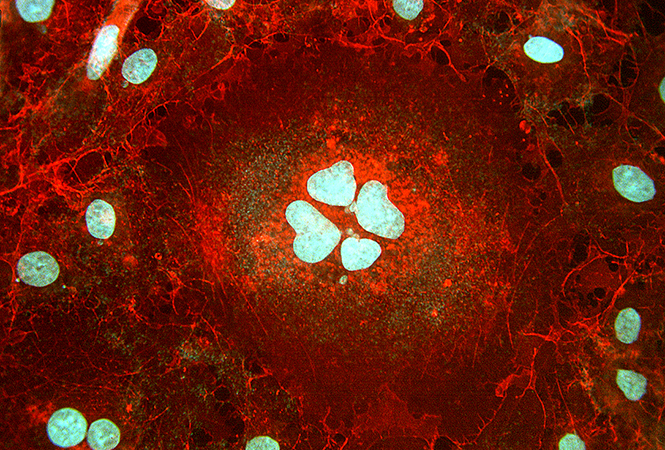
本研究采用乳头顶端的干细胞(SCAPs)。使用碱性磷酸酶(ALP)活性、Alizarin Red S染色、划痕模拟伤口迁移和跨小室趋化实验等方法来评价SFRP2的功能。使用Western blot、实时RT-PCR和ChIP检测评价SFRP2的机制。
结果显示,在炎症和缺氧条件下,SFRP2的过量表达可以增强骨/牙源性分化能力。机制上,SFRP2抑制了Wnt/β-catenin信号通路,进而抑制了核因子kappa B(NFkB)信号通路的靶基因。炎症或缺氧条件下,可通过降低SFRP2启动子的组蛋白甲基化,促进赖氨酸脱甲基酶2A(KDM2A)的表达,抑制SFRP2的转录。此外,蛋白质组学分析表明,SFRP2能促进SCAPs分泌更多的功能性细胞因子,从而提高MSCs的迁移、趋化和成骨/成牙能力。
综上所述,该研究结果表明,SFRP2增强了SCAPs在缺氧和炎症条件下的成骨/成牙分化和旁分泌能力,为促进缺氧和炎症条件下的组织再生提供了一种潜在的细胞因子。
原始出处:
Haoqing Yang, Guoqing Li, et al., Secreted frizzled-related protein 2 promotes the osteo/odontogenic differentiation and paracrine potentials of stem cells from apical papilla under inflammation and hypoxia conditions. Cell Prolif. 2020 Jan;53(1):e12694. doi: 10.1111/cpr.12694.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
81
#CEL#
63
#间充质干细#
64
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
63
#成骨#
111
#PRO#
72
学习了,谢谢分享
119