UROLOGY:经尿道操作会增加尿道狭窄的复杂性吗?
2018-02-23 MedSci MedSci原创
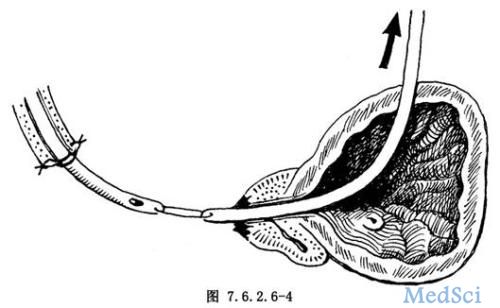
研究人员研究了尿道成形术对尿道狭窄的影响,包括扩张、尿道切开术和支架置换术,这是治疗男性尿道狭窄最常见的方法。
研究人员研究了尿道成形术对尿道狭窄的影响,包括扩张、尿道切开术和支架置换术,这是治疗男性尿道狭窄最常见的方法。
研究人员回顾性地分析了45例在尿道成形术前经尿道治疗的男性的病例记录。研究人员比较了早期诊断与尿道成形术患者的尿道造影结果。在分析中排除了尿道下裂、地衣硬化或既往尿道成形术的男性。研究人员认为,如果尿道成形术中尿道造影的数目和/或长度大于最初诊断或新发现错误通道,则增加复杂性。
其中39例(87%)、32例(71%)和13例(29%)分别接受尿道扩张、尿道切开和尿道支架治疗,39例(87%)发生重复或多种经尿道治疗。22名男性(49%)的复杂性增加,7例(16%)需要的尿道成形术比最初诊断时的尿道造影结果更复杂。增加狭窄的复杂性与尿道切开术(p = 0.03)、尿道支架(p = 0.0002)和重复经尿道治疗(p = 0.01)有显着的相关性。多变量分析显示尿道支架(p = 0.01)和重复尿道治疗(p = 0.01)是增加狭窄复杂性的独立预测因子。
结论
重复的经尿道治疗增加了尿道的复杂性,并且有可能产生副作用。即使是暂时性的尿道支架植入也有可能使狭窄和复杂的尿道成形术复杂化。
原始出处:
Akio Horiguchi.et al.Do Transurethral Treatments Increase the Complexity of Urethral Strictures?UROLOGY.2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#尿道狭窄#
59
#复杂性#
59
#尿道#
69
常见的问题.大道理.学习了!
80
常见的问题
78