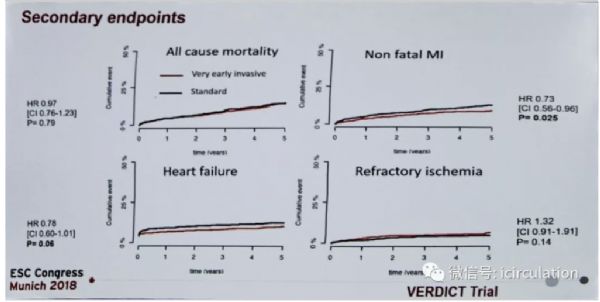
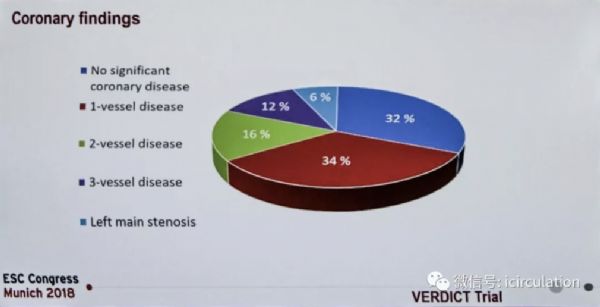
ESC2018丨VERDICT研究:非ST段抬高ACS患者是否应极早期有创评估?
2018-09-04 国际循环编辑部 国际循环
编者按:非ST段抬高急性冠状动脉综合征(NSTE-ACS)患者应何时进行有创冠状动脉评估及介入治疗?这是急诊医生和心脏病介入专家非常关心的临床问题,但尚无确切结论。ESC 2018年会上,丹麦哥本哈根大学Thomas Engstrom教授报告了VERDICT研究的最新研究结果,使参会者对该类患者的有创评估及介入治疗时机有了更多认识。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIC#
51
#非ST段#
76
#非ST段抬高#
68
#ESC2018#
54
#ACS#
56
#ST段抬高#
53
#ACS患者#
76
#ST段#
81
学习,谢谢分享。
80
看看
102