Prostate Cancer P D:较少的经尿道系统活检核心能否与磁共振成像/超声融合活检具有相同的前列腺癌检出率?
2020-08-13 AlexYang MedSci原创
随着活检核心数目的增加,不舒适和并发症的发生率也随着增加。在许多研究中,前列腺癌活检的方法已经由系统生物活检(SB)和靶向生物活检(TB)得到了改善。然而,能够平衡活检并发症和活检准确率的最优前列腺取
随着活检核心数目的增加,不舒适和并发症的发生率也随着增加。在许多研究中,前列腺癌活检的方法已经由系统生物活检(SB)和靶向生物活检(TB)得到了改善。然而,能够平衡活检并发症和活检准确率的最优前列腺取样方法仍旧不明确。
最近,有研究人员探索了一种最优的前列腺癌(PCa)取样方法,且具有更少的SB核心数目。

研究前瞻性的招募了前列腺成像报告至少有1个病变部位和数据系统≥3的患者。每位患者均进行了TB和SB作为参照。假定的取样方案包括TB、SB和TB+nSB(非靶向区域活检)。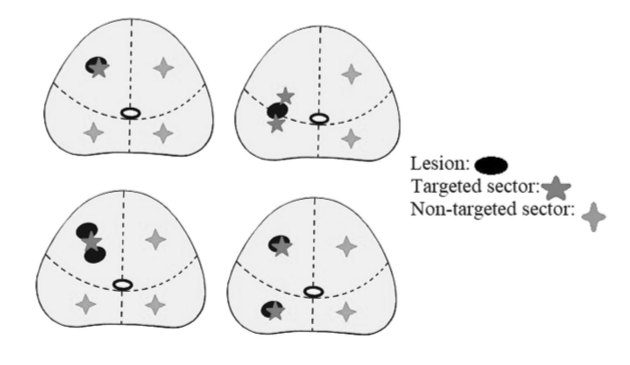
前列腺靶向和非靶向区域
研究发现,在165名患者中,107名(64.8%)患者诊断为PCa,91名(55.2%)患者通过TB+SB诊断为csPCa。在PCa和csPCa患者中,核磁共振成像(MRI)的真阴性案例比例分别为50.5%(54例)和例46.2%(42例),非靶向区域活检的假阴性比例分别为49.5%(53例)和53.8%(49例)。阳性活检案例中的最大癌症比例在这些真假队列中差异显著。而在PCa或csPCa的检出方面,TB+nSB和TB+SB没有差异。
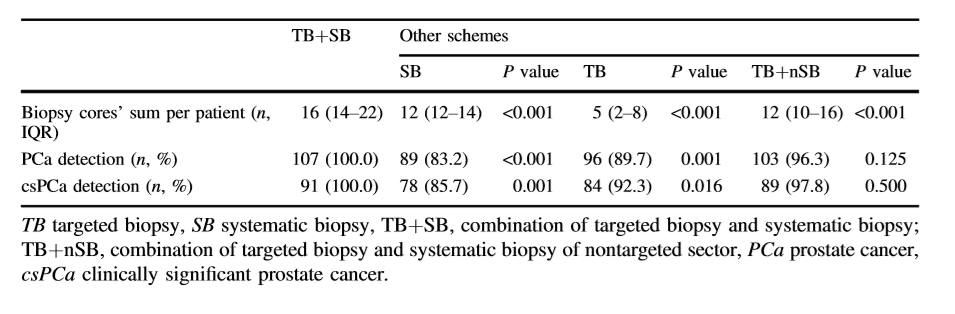
不同方法的前列腺癌检出率比较
最后,研究人员指出,最优的取样方法为TB+nSB,且具有更少的SB核心数目。该方法与标准的TB+SB联用MRI/超声融合活检的检出率相同。
原始出处:
Hua Liu, Mingjian Ruan, He Wang et al. Can fewer transperineal systematic biopsy cores have the same prostate cancer detection rate as of magnetic resonance imaging/ultrasound fusion biopsy? Prostate Cancer P D. 27 July 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Prostate Ca#
92
#尿道#
106
#检出率#
75
#活检#
81
#磁共振#
69
#ROS#
0
#融合#
105
#PRO#
46
学习😊
131
前列腺癌相关研究,学习了,谢谢梅斯
81