ISC 2015:早期血管内治疗可降缺血性卒中患者死亡率(ESCAPE试验)
2015-02-16 高晓方 译 医学论坛网
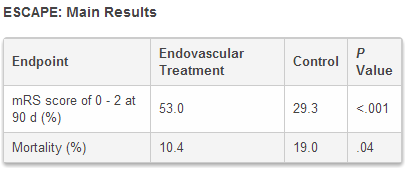
加拿大一项研究表明,在近端血管闭塞的缺血性卒中患者中,早期血管内介入治疗可改善功能转归并降低死亡率。论文2月11日在线发表于《新英格兰医学杂志》(N Engl J Med)。研究于2015年国际卒中大会(ISC2015)上发布。 此项III期试验名为ESCAPE研究,共纳入316例伴有大动脉闭塞的缺血性卒中患者,并随机给予包括tPA在内的标准治疗或标准治疗联合血管内介入。血管内治
加拿大一项研究表明,在近端血管闭塞的缺血性卒中患者中,早期血管内介入治疗可改善功能转归并降低死亡率。论文2月11日在线发表于《新英格兰医学杂志》(N Engl J Med)。研究于2015年国际卒中大会(ISC2015)上发布。[pdf free]
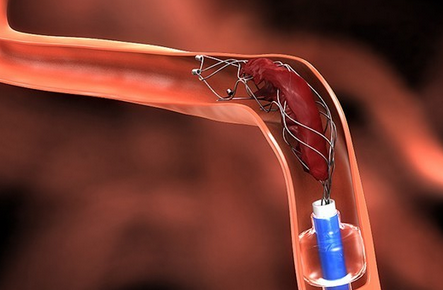
此项III期试验名为ESCAPE研究,共纳入316例伴有大动脉闭塞的缺血性卒中患者,并随机给予包括tPA在内的标准治疗或标准治疗联合血管内介入。血管内治疗不限定特殊装置,但大部分患者应用了可取回支架。利用CT血管造影排除梗塞中心区较大和侧枝循环不佳的患者。主要转归为为改良Rankin量表评分(mRS)。

原始出处:
Goyal M1, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; the ESCAPE Trial Investigators.Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke.N Engl J Med. 2015 Feb 11. [pdf free]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
66
#卒中患者#
55
#CAP#
62
#Escape#
69
#缺血性卒#
51
#缺血性卒中患者#
53
#患者死亡#
47
#缺血性#
56
#SCAP#
61
#ISC#
49