JTO:全基因测序或可指明肺肉瘤样癌靶向及免疫治疗方向
2017-03-21 wrangx 肿瘤资讯
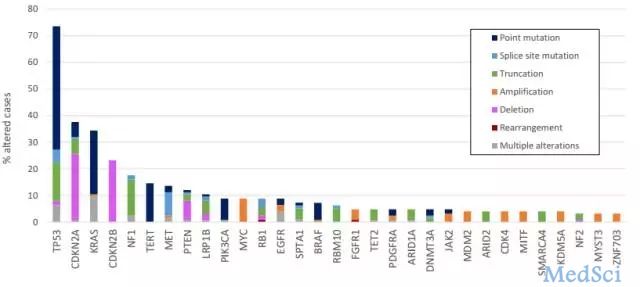
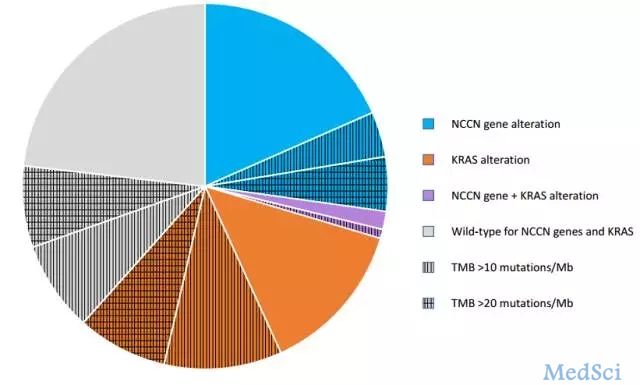
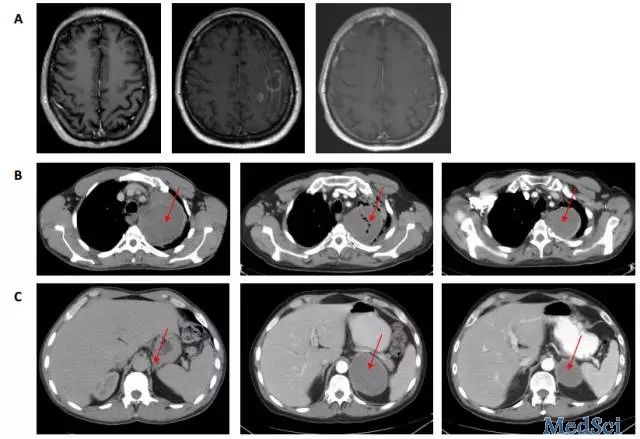
肺肉瘤样癌预后差治疗困难,能否通过基因检测指导精准治疗呢?2017年3月15美国学者B. Schrock 在JTO在线发表肺肉瘤样癌全基因测序文章,发现30%伴驱动基因改变,43%伴中高度肿瘤突变负荷,为免疫治疗和靶向治疗提供依据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肉瘤样癌#
72
学习了分享了
107
学习了分享了
117
学习了,分享了
0
学习了
116
#肺肉瘤样癌#
67
感谢分享一下!
85
谢谢分享,学习了
59
谢谢分享,学习了
51
涨知识,值得学习
57