NEJM:替诺福韦预曝光不能降低非洲女性的HIV-1感染
2015-02-06 Lesley 译 MedSci原创
育龄期女性需要有效的干预措施以防止HIV-1的感染。替诺福韦作为预防HIV-1感染的预曝光能否降低其女性感染率现仍未知,因此Jeanne M等人进行了一项随机、安慰剂对照试验。最新研究结果发表在2015-2-5 NEJM上。 研究者们在2009年9月——2011年6月期间从南非、乌干达和津巴布韦的15个地区筛选12320名符合以下纳入标准的女性:18-45岁非妊娠期、非哺乳期、近期有性交史且
育龄期女性需要有效的干预措施以防止HIV-1的感染。替诺福韦作为预防HIV-1感染的预曝光能否降低其女性感染率现仍未知,因此Jeanne M等人进行了一项随机、安慰剂对照试验。最新研究结果发表在2015-2-5 NEJM上。
研究者们在2009年9月——2011年6月期间从南非、乌干达和津巴布韦的15个地区筛选12320名符合以下纳入标准的女性:18-45岁非妊娠期、非哺乳期、近期有性交史且使用了有效的避孕方法、以及肝肾功血液系统功能未见明显异常的女性。其中7291名女性被排除,最终5029名女性参与该项随机、安慰剂对照试验。参与者按1:1:1:1:1随机分为:1007名口服富马酸替洛抚慰酯TDF(300mg)、1003名口服联合替诺福韦和恩曲他滨TDF-FTC(300mg TDF+200mg FTC)、1009名口服安慰剂组、1007名使用1%替诺福韦凝胶阴道给药组和1003名阴道凝胶安慰剂组共5组。用药方案为每日服用。研究者们每个月行一次HIV-1检测,每季度行一次血浆TFV水平检测。
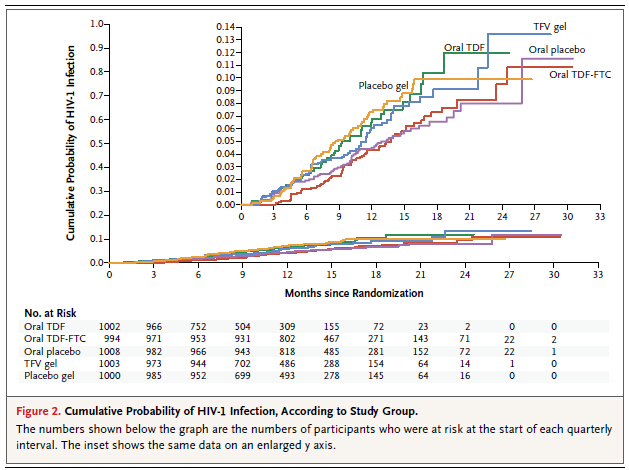
该项研究结果指出:试验设计的三种给药方案均没有显著降低非洲育龄期女性HIV-1的感染。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








赞
146
已阅
149
#替诺福韦#
62
预防HlV还有一段话
143